-
PDF
- Split View
-
Views
-
Cite
Cite
Mina Azer, Alejandro-Daniel Lira-Schuldes, Hans-Uwe Volkers, Internal herniation of the caecum and the ascending colon through the foramen of Winslow, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa029, https://doi.org/10.1093/jscr/rjaa029
Close - Share Icon Share
Abstract
We are reporting a case of internal herniation of the bowel through the foramen of Winslow. This is a very rare condition that prompts an urgent operative intervention due to its potential fatal complications, as it is usually accompanied by bowel strangulation and ischemia. Due to the vague clinical picture, the diagnosis only reached using imaging techniques such as computed tomography or as a surgical surprise during the operation. Key aspects of surgical interventions are hernia reduction, bowel resection in case of non-viable ischemic bowel and the highly debatable recurrence prevention maneouvres.
INTRODUCTION
The lesser peritoneal sac is a potential space posterior to the stomach. It communicates with the greater peritoneal sac via the epiploic foramen, which is also known as the foramen of Winslow after the Danish-born French anatomist Jacques-Bénigne Winslow (1669–1760). To understand the anatomy of the foramen of Winslow, you can imagine yourself entering the lesser sac. You are stepping on the peritoneal covering of the inferior vena cava and passing under the free boarder of the lesser omentum, which harbors the common hepatic artery, the portal vein and the common bile duct. To the right you can touch the first part of the duodenum and to the left the liver.
We are reporting a rare case of internal herniation of the caecum and the ascending colon through the foramen of Winslow.
CASE REPORT
A male patient, 69-years old was presented in our emergency department complaining of severe abdominal pain. The patient described the pain as paroxysmal cramps, which starts at the lower abdomen then radiate to the epigastrium and to the back. The complaint began approximately 24 h before the admission and was associated with distention and mild nausea. Vomiting, fever or altered bowel habits were not reported. The patient suffers from obesity, arterial hypertension, metabolic syndrome and uncomplicated sigmoid diverticulosis. He underwent a laparoscopic Nissen fundoplication 2 years ago. Few weeks after this operation, he suffered a migrated wrap that was surgically repaired. Clinical examination revealed abdominal tenderness without guarding or rigidity. Intestinal sounds were present but weak. Laboratory tests showed no significant abnormalities.
In absence of signs of peritonitis, we decided to proceed with further investigations. Abdominal sonography was hindered by distention. Contrast-enhanced computed tomography (CT) of the abdomen showed a single-intestinal loop, which appeared to be distended and trapped behind the stomach. As the possibility of internal herniation rose, we scheduled the patient for an urgent abdominal exploration.
The operative findings confirmed the radiological interpretation. The operator could retract the twisted ascending colon and caecum out of the lesser sac through the foramen of Winslow, only after decompression of the strangulated bowel, via suction of gas and fluid content through a small incision. The initially congested herniated colon regains normal appearance soon. In the absence of permanent ischemic changes, the operator opted for minimal intervention. Without colectomy, the abdomen was temporary closed, with a second-look planned after 24 h, which revealed viable intestine with no signs of intestinal obstruction. The patient stayed in the intensive care unit for 2 days and was discharged at the seventh postoperative day after he showed good recovery and uneventful hospital stay.
DISCUSSION
While it represents to hepatobiliary surgeon’s an important landmark, the foramen of Winslow is rarely encountered by general surgeons in the context of internal hernia. Adult internal hernia is considered to be a rare condition that represent only 0.2–0.9% of hernias [1]. Internal herniation through the foramen of Winslow represents only 8% of internal hernias [2], which render it a very rare condition, almost only addressed in literature through case studies. Another factor that makes its management challenging is the vague nature of the initial clinical picture. The patient is usually presented with diffuse or upper abdominal pain with neither signs of peritonism nor absolute intestinal obstruction [3]. This in turn, leads to a significant delay in the therapeutic decision making causing the relatively high-reported mortality rate of ~50% [2].
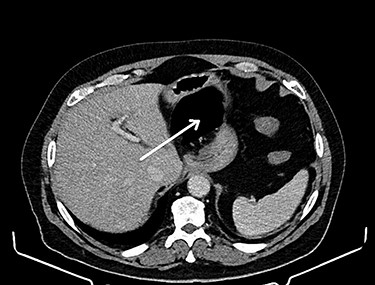
CT of the abdomen is considered the gold standard of the diagnosis of the internal hernia through the foramen of Winslow. The most prominent feature is the presence of intestinal loops between the inferior vena cava and portal vein [4] (see Fig. 1). Another classic feature is the presence of distended intestinal loops posterior to the stomach, which is displaced along with first and second part of the duodenum to the left [5] (see Fig. 2).

Intestinal loops (arrow) between the inferior vena cava and portal vein.
As any rare condition, there is no general consensus regarding a standard management of internal hernia through the foramen of Winslow. The only widely accepted opinion is the indication of an urgent surgical intervention due to the risk of strangulation and acute intestinal ischemia [6]. Here, we can discuss three key aspects of surgical interventions: hernia reduction, bowel resection and recurrence prevention.
Reduction of the hernia could be challenging due to the marked distention of the entrapped intestinal loop (see Fig. 3). Bowel decompression through needle puncture or a small incision was frequently described to facilitate the reduction [7]. Another accepted option is widening the foramen of Winslow to aid reduction using Kocher’s maneuver [8]. The duodenum could be mobilized to the left by incising the peritoneum at its right edge. This technically demanding maneuver is reserved as a last resort. Bowel resection is indicated in case of a non-viable strangulated bowel. On the other hand, viable bowel is frequently reported, where no resection was needed [9]. Right hemicolectomy was described along with caecopexy and narrowing of the foramen Winslow as recurrence prevention maneuvers [7]. These maneuvers are highly debatable due to their added risk of postoperative morbidity in the lack of a hard evidence of recurrence, which remains more of theoretical risk [10].
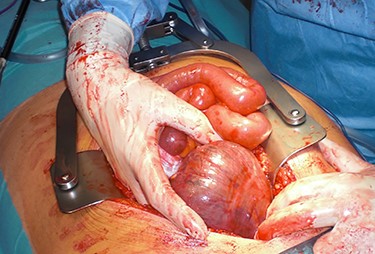
Herniated caecum and ascending colon through the foramen of Winslow.
In conclusion, internal herniation through the foramen of Winslow is a very rare condition. Yet, it should not to be missed due its fatal potential. In the presence of the characteristic features of the CT imaging, urgent surgical intervention should follow.



