-
PDF
- Split View
-
Views
-
Cite
Cite
Li Lian Kuan, John Isherwood, Cristina Pollard, Ashley Dennison, A unique case of a double common bile duct with ectopic drainage into the gastric antrum: a case report and review of the literature on double duct variants, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa028, https://doi.org/10.1093/jscr/rjaa028
Close - Share Icon Share
Abstract
Variants of hepatic duct anomalies are widely discussed in the literature. Duplication producing a double and/or aberrant extrahepatic bile duct is one of the rarest congenital variants that have been sparingly reported. A 71-year-old female presented with right-sided abdominal pain. Computerized tomography demonstrated an enhancing soft tissue thickening in the gastric pylorus with extension into the left lobe of the liver and invasion of the left intrahepatic bile ducts and dilatation of the left intra- and extrahepatic biliary tract. Further examination led to a diagnosis of a double common bile duct with ectopic drainage into the gastric antrum. Recognition of this rare anomaly is of great importance because of the implications in respect of concomitant pathology, the potential short- and long-term sequelae and crucially for operative planning. Failing to appreciate the extent of anomalies may result in significant complications with the attendant morbidity.
INTRODUCTION
Although anatomical variants of the hepatic artery have been exhaustively described in the literature descriptions of anomalous hepatic and common bile ducts are less frequently reported. Duplication of the extrahepatic bile duct, a double (DCBD) or accessory/aberrant common bile duct (ACBD), is one of the rarest congenital variants and has been sparingly reported. Accurate, widespread knowledge of the biliary anatomy and its variations is essential for preoperative planning, to minimize postoperative complications and of its association with concomitant pathology and the related sequelae.
CASE REPORT
A 71-year-old female presented with right upper quadrat (RUQ) pain associated with vomiting. She has no significant past medical or surgical history. Laboratory results revealed a normal white cell count and liver function tests but a raised C-reactive protein.
Computerized tomography demonstrated an enhancing soft tissue thickening in the gastric pylorus with soft tissue extension into the left lobe of the liver, invasion of the left intrahepatic bile ducts with obstruction and dilatation of the left sided intra- and extrahepatic biliary tract (Fig. 1). Oesophagogastroduodenoscopy (OGD) showed a pre-pyloric fistula (Fig. 2).
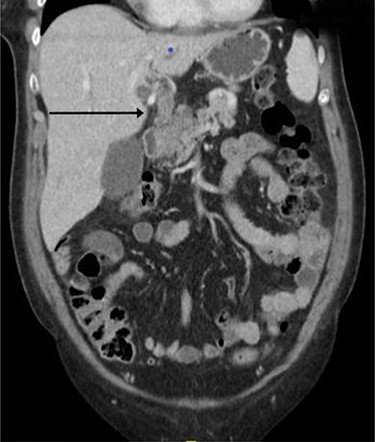
Computed tomography imaging showing continuous tubular structure extending from the left hepatic lobe to the stomach.
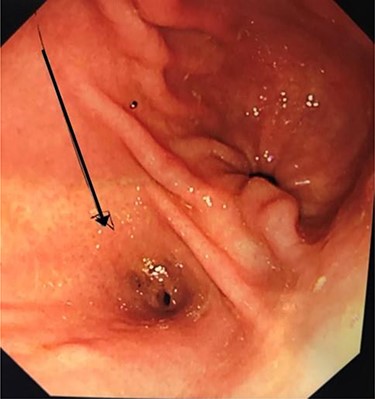
Oesophagogastroduodenoscopy (OGD): pre-pyloric fistula—ectopic opening of the ACBD.
Further examination led to a diagnosis of DCBD with a separate left intra- and extrahepatic bile duct with ectopic drainage into the stomach. Magnetic resonance cholangiopancreatography (MRCP) revealed marked left intrahepatic duct (IHD) dilatation. The left IHDs were draining via an aberrant extra-hepatic bile duct into the pre-pyloric region. The left and right hepatic ducts did not communicate. It also demonstrated pancreatic divisum and multiple side branch intra-ductal papillary mucinous neoplasms (IPMN) (Fig. 3). Endoscopic retrograde cholangiopancreatography (ERCP) confirmed the MRCP findings but also revealed an intraluminal-filling defect in the left IHD (Figs 4 and 5).
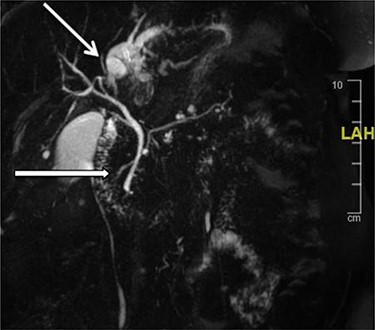
MRCP: open arrow—the left IHDs drain via an aberrant (left) extra-hepatic bile duct into the pyloric region without communication with the (right) intra- and extra-hepatic bile ducts. Closed arrow—pancreatic divisum and side branch IPMN.

ERCP: cannulation via the major papilla orifice into the CBD draining the right IHDs. There was no communication between the ACBD and the right IHDs.

ERCP: cannulation via the pre-pyloric fistula opening. Contrast outlining the ACBD and the left IHDs.
She underwent a left hemi-hepatectomy and a wedge excision of the antrum of the stomach. Intraoperative examination confirmed the radiological findings (Figs 6–8). There were an atrophic left liver lobe and a dilated ACBD draining segments 2–4. The left portal vein crossed anteriorly to the ACBD with the left hepatic artery (LHA) lying medial to it. An accessory LHA was also present within the hepato-gastric ligament. Postoperative recovery was uneventful. Histology showed intraductal papillary neoplasm of the bile duct (IPN-B) with low-grade dysplasia involving both the intra- and extrahepatic bile ducts.
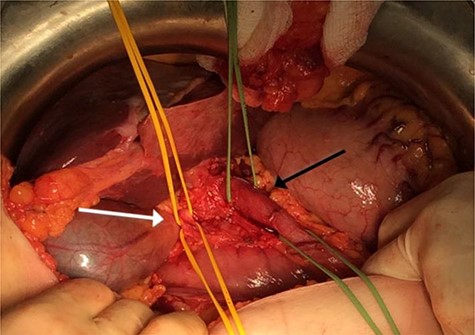
Intraoperative image showing a dilated ACBD draining segments 2–4 (black arrow) and the right sided non-dilated CBD (white arrow).
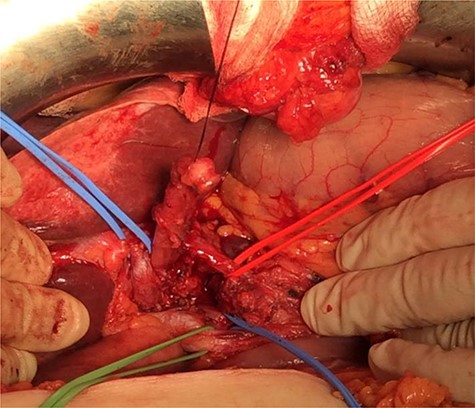
Intraoperative image. Blue sling: portal vein. Green sling: right extra-hepatic bile duct. Black sling: ACBD.

DISCUSSION
DCBD is an extremely rare anomaly and is defined as a congenital deformity in which two patent bile ducts open separately into the gastrointestinal tract and may drain into different parts of the stomach, duodenum and pancreatic duct.
Vesarius in 1543 first described duplication of the CBD. In the fourth week of embryological development, the hepatic diverticulum rapidly proliferates into the septum transversum and divides into two parts; the pars hepatica that forms the liver and hepatic ducts, and the pars cystica that develops into the gallbladder and cystic duct [1]. Deviation from this normal pattern of development results in a variety of associated anomalies.
The incidence of congenital anomalies of the extra-hepatic biliary system varies between 0.58 and 47.2% [2]. Yamashita observed 47 cases and found the main presenting symptoms were epigastric or RUQ pain (80.1%), ratio of female to male was 1.6:1, and mean age of 46.1 years old [3]. In 1.7% of cases, DCBD was reported to arise from the right liver lobe and 2.2% from the left side [4].
DCBD was first classified by Goor and Ebert into seven different configurations based on their anatomical structure in 1972. Saito et al. [5] modified the classification describing four configuration types without regard to the anatomical opening. In 2007, Choi et al. proposed a classification based on morphology with the addition of a fifth type of anomaly which does not take into account the site of the opening of the aberrant CBD. He described five types: type I: the septum dividing the bile duct lumen, type II: the bifurcation of the distal bile duct and each channel draining independently into the bowel, type III: duplicated extrahepatic bile ducts (a) without or (b) with intrahepatic communicating channels, IV: duplicated extrahepatic bile duct with extrahepatic communicating channel or more than one communicating channels, V: single biliary drainage of double bile ducts without (a) or with (b) communicating channels [6]. According to this classification, the case we have described is type IIIa. In total, 47 cases of DCBD reported in Japan between 1968 and 2002, were ~50% of type III [3].
It is important to recognize this anomaly because of its clinical implications and association with an aberrant pancreatico-biliary junction, choledochal cysts, biliary atresia and upper gastrointestinal cancers [7]. Furthermore, DCBD can cause complications including calculus formations, cholangitis and cholecystitis. This anomaly was reviewed in the oriental population and observed that cholelithiasis was found in 27.7%, choledochal cyst in 10.6%, pancreatobiliary maljunction (PBM) in 29.8% and malignancy in 25.5% [3].
The feared sequela of DCBD is carcinogenesis. The site of opening of the ACBD is relevant as biliary and pancreatic reflux with chronic inflammation is associated with site-specific malignancies [7]. Concomitant gastric cancer was frequently noted when the ACBD opened into the stomach and cancer of the biliary system when the ACBD opened into the second part of the duodenum or the pancreatic duct [3].
Kondo [8] reported two cases with DCBD with ectopic drainage into the stomach associated with gastric carcinoma and a possible correlation between direct flow of bile juice into the stomach. DCBD is also associated with a higher risk of bile duct cholangiocarcinoma due to the chronic cholangitis caused by constant pancreatobiliary reflux which may result in dysplasia with or without intestinal metaplasia, and subsequently invasive carcinoma [9]. In our case, IPN-B was the final diagnosis, which is a precursor for intrahepatic cholangiocarcinoma. Fan et al. [10] did not find any Type I cases presenting with malignancy, as type I has no anomalous PBM and very low incidence of malignancy, simple resection of the septum is usually sufficient. For types II, III and IV, complete resection of the ACBD that opens into the stomach or pancreas is recommended followed by strict surveillance. The management strategy for type V DCBD remains unclear.
CONCLUSION
Accurate and detailed knowledge of the biliary anatomy and its variations are essential for preoperative planning to minimize postoperative complications. Awareness of the possibility of these major and complex anomalies should increase their reported incidence and decrease the potentially severe associated morbidity and mortality. Where the anomalies are extensive, associated with ectopic drainage and chronic reflux, the associated risk of malignancy must be appreciated, and the surgical procedure and consequent surveillance modified to obviate the consequences.
Conflict of interest statement
None declared.
Disclosure
Non-financial support disclosed.



