-
PDF
- Split View
-
Views
-
Cite
Cite
Wen Jie Choy, Ganeshwaran Shivapathasundram, Lachlan Cassar, Ralph J Mobbs, Dynamic myelopathy as a result of C1 posterior arch aplasia and os odontoideum. A case report, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa019, https://doi.org/10.1093/jscr/rjaa019
Close - Share Icon Share
Abstract
The atlas (C1) and axis (C2) have distinct morphologies to support the skull and facilitate head rotation and neck flexion. Congenital defects of C1 posterior arch are rare. We present a case of a 59-year-old man with both an absent C1 posterior arch with concomitant os odontoideum. The patient presented with neck crepitus, moderate neck pain and progressive worsening upper limbs paraesthesia and pain. Computed tomography (CT) revealed non-union between the odontoid process and body of axis as well as absence of C1 posterior arch. An occiput C0–C3 fusion was performed. The patient’s symptoms improved significantly, and he is functioning well at 12 months. CT showed solid fusion without implant migration. Concomitant os odontoideum with aplastic C1 posterior arch is rare with limited evidence to guide management. Posterior fixation and fusion may be a potential solution to prevent dynamic compression, thereby preventing further myelopathy and related complications.
INTRODUCTION
Named after the Greek god who held up the celestial sphere, the atlas (C1) holds up the human skull. Together the atlas and axis form the crucial connection between skull and spine. They facilitate the important function of head rotation. The anatomy of the atlas (C1) and axis (C2) is therefore unique and distinct from the other vertebrae of the spine [1, 2]. Both atlas and axis are crucial for stability and motion. Multiple ligaments including the atlanto-occipital ligaments, the cruciate ligament and the alar ligaments ensure smooth motion while not compromising stability [1, 3].
Congenital defects of the posterior arch of atlas (C1) are rare. We describe a case of a 59-year-old man with both an absent C1 posterior arch and concomitant os odontoideum causing atlanto-axial instability and a dynamic myelopathy. This case highlights the importance of considering congenital anomalies of the occipitocervical junction as these can be a cause of atlanto-axial instability and myelopathy.
CASE REPORT
A 59-year-old right-hand-dominant Australian male presented with a 3-year history of neck crepitus, moderate neck pain and progressive dysfunction including worsening upper limbs paraesthesia and pain. He was in remission from Hodgkin’s lymphoma 5 years ago post-stem cell and chemotherapy. He was a smoker.
On examination, he had a robotic gait and signs of early cervical myelopathy. Cervical movement was severely limited with rotation at 10–15 degrees, and flexion–extension similarly limited. Deep tendon reflexes were reduced in the upper limbs, increased in the patellar ligament and reduced in the Achilles tendon possibly resulted from chemotherapy induced peripheral neuropathy.
Computed tomography (CT) demonstrated non-union between the odontoid process and body of axis, as well as absence of the posterior arch of atlas (Fig. 1A). Magnetic resonance imaging revealed myelomalacia at the level of non-union likely due to repetitive dynamic compression (Fig. 1B). Flexion–extension X-ray films confirmed significant distraction and forward translation at the atlanto-axial joint (Fig. 2).
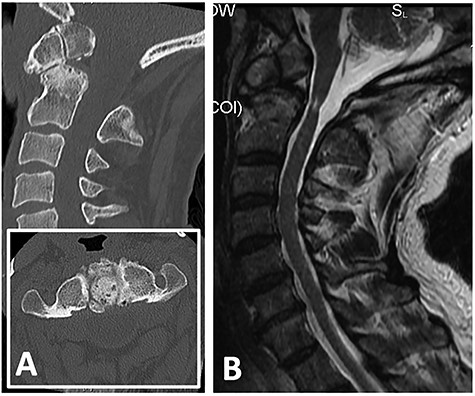
(A) CT showing non-union between odontoid process with body of axis (C2) and absence of posterior arch of atlas (C1); (B) T2-weighted MRI revealing cord signal change and atrophy at level of C1/2 suggestive of myelomalacia.
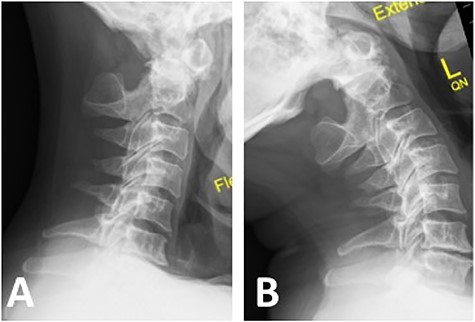
Note the absence of posterior arch of atlas (C1); (A) flexion X-ray revealed antero-inferior translation of atlas (C1) on axis (C2); (B) extension X-ray revealed postero-superior translation of atlas (C1) on axis (C2).
Due to the atlanto-axial instability causing dynamic myelopathy, fusion was the best solution to prevent further dynamic injury to the spinal cord. However, the patient’s aberrant anatomy (absence of posterior C1 arch) prevented the placement of C1 pedicle screws. Hence, an occiput C0–C3 fusion was planned to stabilize his craniocervical junction.
The patient was positioned prone on a Wilson frame with his head secured in a slightly extended position using a Mayfield clamp. The position was confirmed with lateral fluoroscopy. A midline incision was made and standard subperiosteal dissection of the occiput and cervical spine was performed. Intra-operative radiography confirmed the absence of C1 posterior arch. Bilateral C3 lateral mass screws and C2 pars/pedicle screws were inserted. The occipital plate anchored with four bicortical screws was connected to the screws using titanium rods and secured with cross linking. The exposed occiput and lamina of C2 and C3 were decorticated and autograft from C2 and C3 spinous processes was mixed with demineralized allograft (Allovance, Australian Biotechnologies, Sydney, Australia).
The patient was prescribed a cervical orthosis (Miami J collar) for 3 months post-operatively. Day 1 post-operative CT demonstrated satisfactory hardware positioning. Follow up X-ray at 4 weeks and CT at 12 months demonstrated good implant positioning without evidence of migration (Fig. 3). Neck pain and upper limb symptoms were significantly improved, and patient has been functioning well.
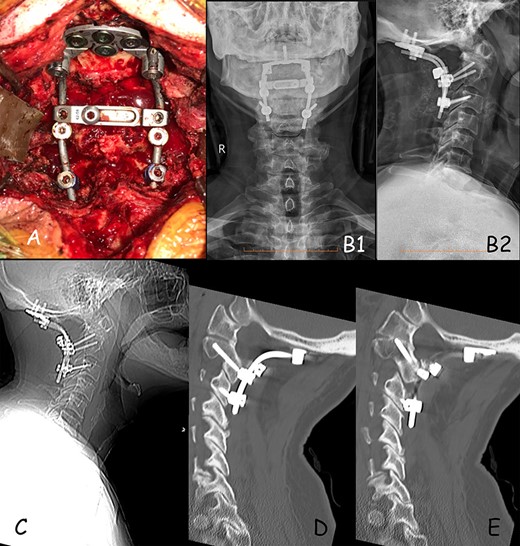
(A) Intra-operative positioning of occipital plate and screws construct. (B) 1-month post-op X-ray, (B1) anterior–posterior and (B2) lateral X-ray. (C) 12-months post-op lateral X-ray showing good positioning of construct. (D) Sagittal CT demonstrating good positioning of construct on the right side. (E) Sagittal CT demonstrating good positioning of construct on the left side.
DISCUSSION
Embryologically, the atlas is formed by three primary ossification centres. At the seventh week of gestation, two lateral centres extend posteriorly to form the posterior C1 arch. In roughly 2% of population, a fourth ossification centre which forms the posterior tubercle is present at age 2 years [4]. The anterior arch, however, does not develop until after birth with the anterior ossification centre(s) seen in the first year of life radiologically. Fusion of the anterior arch occurs from ages 3 to 5 years and can occur up to 9 years [1, 5].
Normal axis development originates from multiple ossification centres. The dens arises from the fourth occipital, and the first- and second-cervical sclerotome. The body of the dens, originally a part of the centrum of the atlas, detaches and fuses with the axis between gestation weeks 6 and 7. Postnatally, the dens remains separated from the body by a neurocentral synchondrosis. This vestigial disc disappears mostly at the age of 8 years [3, 6]. However, the synchondrosis is not the base of the dens [6]. The lack of trabecular bone at the base makes it an area of weakness [3].
Congenital hypoplasia of the C1 posterior arch are classified into five categories by Currarino et al.’s based on the degree of anomaly, which stems from embryological developmental defect. This patient’s complete lack of posterior C1 arch would be classified as a type E (Fig. 4) [7]. Although sparse, findings of patients with anomalies in their C1 arches are usually incidental. Patients with Types C and D anomalies are at higher risk of myelopathy due to the presence and dynamic compression of posterior tubercle, which may cause impingement of the spinal cord during neck extension [8, 9].
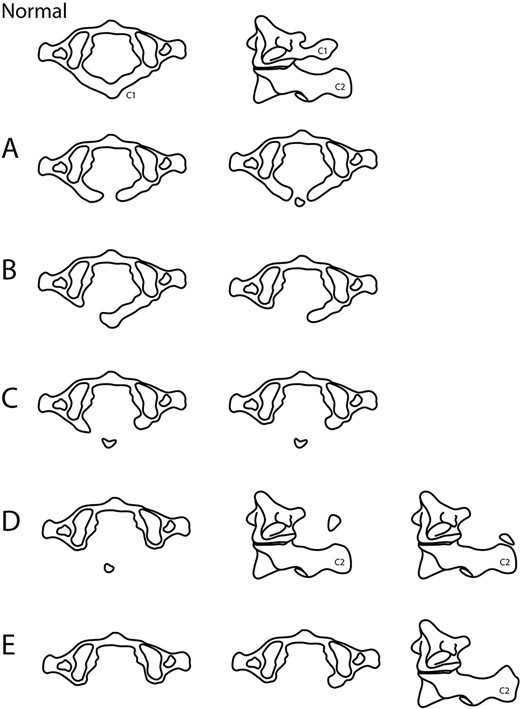
Currarino et al.’s classification of C1 hypoplasia. (A) Failure for midline fusion of both ossification centres of C1 posterior hemiarches; (B) Unilateral defect in one C1 posterior arch; (C) Bilateral clefts with preservation of most dorsal aspect; (D) Absence of C1 posterior arch (usually asymmetrical defects) with an unattached posterior tubercle of C1, which position may be well above or in contact with C2 spinous process; (E) Complete absence of C1 posterior arch and tubercle, spinous process of C2 may also be hypertrophied.
Os odontoideum is another incidental radiological finding involving the dens of C2 with a debatable aetiology (congenital or traumatic). Incomplete ossification of the synchondrosis separating the dens and C2 body, genetics are different theories that associate os odontoideum to congenital causes [3, 10]. On the other hand, due to late ossification across the synchondrosis during development, early childhood bony or ligamentous injury can result in separation of the dens from the body. Other traumatic theories include fracture of the cartilage dens in utero, repeated microtrauma or unrecognized trauma resulting in stress fractures and anatomically comprise mainly of trabecular bone in the base [3].
Due to the rarity of hypoplastic arch and os odontoideum, limited evidence is available to guide the management. The general consensus is surgical fixation and stabilization if dynamic myelopathy is present [11]. To prevent further complications/damage, a C0–C3 posterior fusion was carried out to stabilize the craniovertebral junction. Decompression was not carried out in this case as there are no signs of stenosis demonstrated in neutral imaging (Fig. 1B).
Conflict of interest statement
None declared.



