-
PDF
- Split View
-
Views
-
Cite
Cite
Han N Beh, Yuni F Ongso, David B Koong, Transmesocolon internal hernia masking as simple sigmoid volvulus, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa017, https://doi.org/10.1093/jscr/rjaa017
Close - Share Icon Share
Abstract
Transmesocolon internal hernias are very rare causes of bowel obstruction. Transmesenteric internal hernias normally associated with small bowel. It can be challenging to diagnose transmesocolon internal hernia hence we present a 93-year-old patient who was misdiagnosed with simple sigmoid volvulus on CT abdomen. She underwent endoscopic colonic decompression. Patient continued to deteriorate in the ward, and CT abdomen was repeated; it revealed the cause of the sigmoid volvulus was due to a defect through transverse mesocolon resulting in internal hernia. Patient was diagnosed with transmesocolic internal hernia with sigmoid volvulus. Patient underwent emergency laparotomy and Hartmann procedure. Transmesocolic internal hernia can be easily missed and needs to be considered when diagnosing patients with large bowel volvulus or obstruction.
CASE REPORT
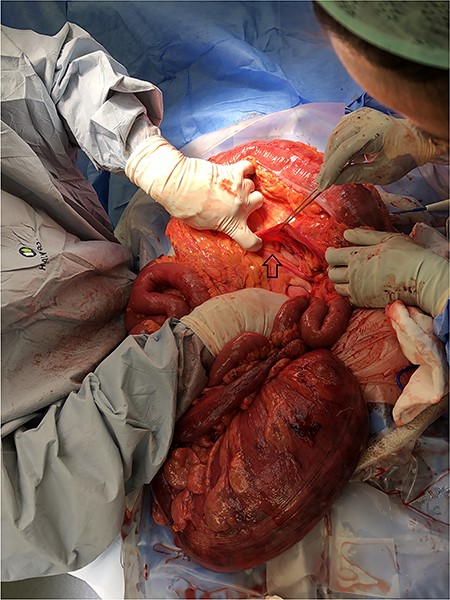
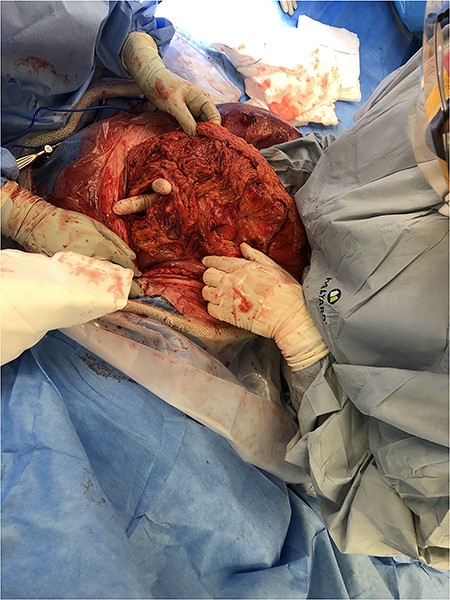
A 93-year-old patient who has history of recurrent sigmoid volvulus presented with a week of abdominal distension and bowels not working. Initial blood test revealed that she has white cell count 11.3 × 109/L, CRP 12 and lactate of 1.9. CT abdomen was performed on admission showed features of sigmoid volvulus. Patient was booked for flexible sigmoidoscopy to decompress the sigmoid volvulus. Flexible sigmoidoscopy revealed that there was significant mucosal necrosis of the sigmoid colon. A diagnostic laparoscopy was performed to determine the severity of necrosis. Laparoscopy reported that the sigmoid colon was oedematous but no signs of transmural necrosis. Patient was kept in the hospital for observation but there were no signs of improvement. Day 4 of the admission, patient continues to deteriorate clinically and had a medical emergency team response call for worsening pain and hypotension, and a repeat CT abdomen was performed. The images were consistent with sigmoid volvulus through transmesocolon defect resulting an internal hernia (Figure 5–7). The patient had emergency laparotomy. The sigmoid colon was found to be in the supracolic compartment and required decompression prior to reduction (Figure 1–4). There was transmural necrosis close to the rectosigmoid junction. Patient underwent Hartmann procedure. Patient recovered well postoperatively and discharged to home.
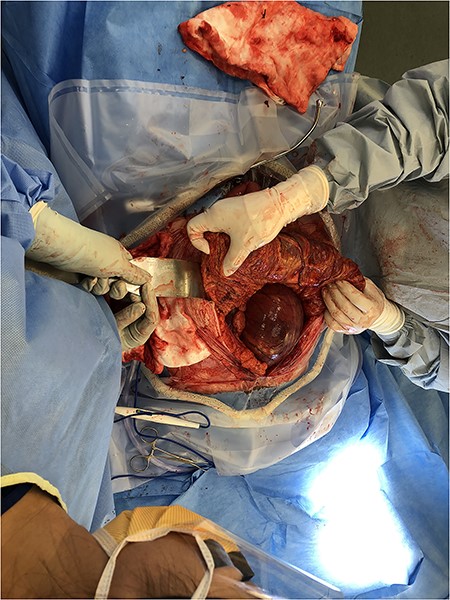
Sigmoid Volvulus pre-decompression within the supracolic compartment.


CT pm sagittal view showing sigmoid colon herniating through trasn-mesocolon defect.

CT on coronal view showing sigmoid colon in the supracolic compartment.

CT on axial view showing twisting of sigmoid colon resulting in volvulus.
DISCUSSION
An internal hernia is the protrusion of abdominal organ through normal or abnormal mesenteric or peritoneal aperture [1]. An internal hernia can be acquired as a result or trauma or surgical procedure. In the broad category of internal hernias, there are several main types based on their location, as traditionally described by Meyers. These consist of paraduodenal (53%), pericaecal (13%), foramen of Winslow-related (8%), transmesentric and transmesocolic (8%), intersigmoid (6%) and retroanastomotic (5%), with the overall incidence of internal hernia being 0.2–0.9%.
Transmesocolic hernias are more likely than other subtypes to develop volvulus and strangulation, or ischemia, the reported incidence of which are as high as 30 and 40%, respectively, with mortality rates of 50% for treated groups and 100% for non-treated subgroups [2]. Sigmoid volvulus is a common general surgery emergency. It accounts for 3–5% of intestinal obstruction in USA, Europe and Australia. Congenital transmesenteric internal hernias are mainly small bowel and majority involving sigmoid mesocolon [3–6].
Internal hernias can often be difficult to diagnose purely based on clinical and examination findings. Simple plain X-ray will likely diagnose sigmoid volvulus but unable to detect internal hernias. CT has been an important diagnostic tool to identify internal hernias. We often diagnose sigmoid volvulus rapidly on imaging and proceed to manage it endoscopic decompression. The patient had recurrent presentations and was diagnosed with redundant sigmoid colon that is predisposing her to have recurrent sigmoid volvulus. It is crucial that imaging needs to be examined carefully and to avoid missing transmesocolic defect. The transmescolic defect was the actual cause of internal hernia. It is uncommon to have sigmoid colon through the defect and appearing as sigmoid volvulus. The previous CT imaging was carefully examined and revealed that the transmesocolon defect was present 1 year ago for the previous presentation of sigmoid volvulus. It is likely that the cause of her presentation was due to the transmecolon defect internal hernia.
In conclusion, transmesocolic internal hernias are exceedingly rare and we need to be vigilant in reviewing patient’s investigation. This could be easily missed as a simple sigmoid volvulus and the management pathway is different from a sigmoid volvulus due to transmesocolic defect. Patient’s failure to progress could mean that sigmoid volvulus did not completely resolve post-decompression. It is crucial to keep in mind that a transmesocolic internal hernia can mask as a simple sigmoid volvulus.



