-
PDF
- Split View
-
Views
-
Cite
Cite
Ângela Ferreira, Sílvia Dionísio, Eduardo Ventura, Rute Saleiro, Carlos Monteiro, Parapharyngeal schwannoma—a challenging case report, Journal of Surgical Case Reports, Volume 2020, Issue 3, March 2020, rjaa048, https://doi.org/10.1093/jscr/rjaa048
Close - Share Icon Share
Abstract
Parapharyngeal space primary neoplasias are infrequent findings in clinics, and schwannoma derived from a peripheral nerve is even rarer in this anatomic area [1]. The presented case is a patient who was referred to our department with a 3 months progressive soft palate enlargement without related symptoms. The challenge, in these cases, due to the anatomic complex area, is to catch a suitable approach to remove the tumor, according to dimension and surrounding structures. Prognosis and follow-up will depend on histopathologic evaluation.
INTRODUCTION
Deep in the neck, a virtual space can be found, the parapharyngeal space, where neoplasms can slowly grow and cause a wide range of symptoms. Tumors in this area are not common despite the complexity of anatomical structures [1].
Schwannomas or neurilemmomas have their origin in Schwann cells, which sheathe a normal nerve fiber. Schwannomas are slow-growing tumors, usually asymptomatic until they are markedly large and they displace medial and anterior anatomic structures such as vessels or soft structures. We should suspect malignancy when pain or nerve paralysis [3].
We present a patient with a parapharyngeal space mass, which was surgically removed via a transcervical approach with lip-split and lateral mandibulotomy.
CASE REPORT
We present a case of a middle-aged woman referred to our Maxillofacial Department with progressive asymptomatic growth of a mass in the right soft palate noticed 1 month before. She denies having a sore throat, a change in voice quality, dysphagia, trismus or nasal obstruction.
The patient underwent a CT neck revealing a bulky oval right parapharyngeal lesion, well-defined, with 41 × 51 × 54 mm (Fig. 1). The mass remodeled the pterygoid processes and mandibular ramus, extending up to the skull base, increasing oval foramen without intracranial invasion. It deformed the oropharyngeal and nasopharyngeal cavities without airway compromise.
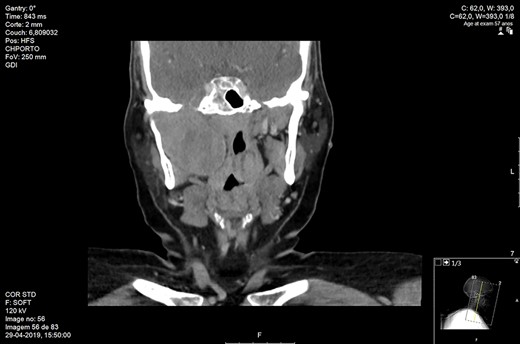
Maxillofacial coronal CT. Right parapharyngeal mass with 54 mm of craniocaudal dimension and 51 mm of transversal dimension.
In order to clarify the diagnosis, a biopsy was performed under local anesthesia. Histologic examination revealed narrow, elongated and wavy cells with tapered ends interspersed with collagen fibers, without mitotic cells, atypia or necrosis. This was suggestive of peripheral nerve sheath proliferation.
It was planned a surgical excision of the tumor under general anesthesia. The access was gained with a right submandibular incision extending to the lip and intra-oral cavity with marginal nerve preservation. Submandibular gland was removed and lingual nerve spared. Then, the flap was raised with mandibular exposure, and ramus mandibulotomy was performed to access the tumor area (Fig. 2). The tumor was reached and removed en bloc with the capsule leaving all the surrounding structures undamaged (Fig. 3). Mandible was reconstructed with a bended plate and six screws. There were no complications post-operatively. She was discharged 10 days after surgery.
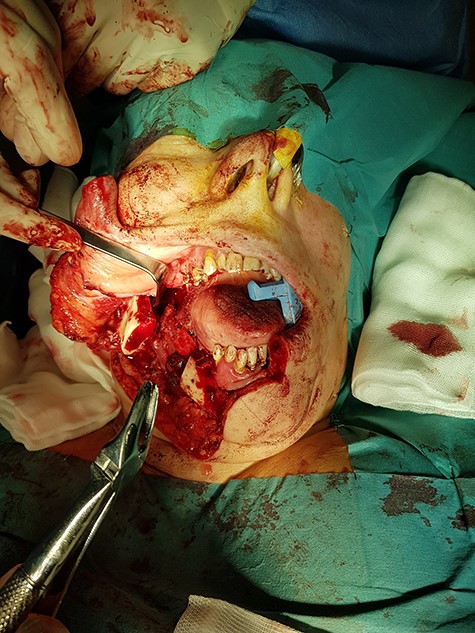
Intraoperative removal of the mass. Transcervical approach with lip-split and mandibulotomy.

Histological examination of the operating material revealed a tumor formed by spindle Schwann cells (S100+), exhibiting hypo and hyper cellular areas. There were no mitosis figures or necrosis (Fig. 4), compatible with nerve sheath neoplasia.
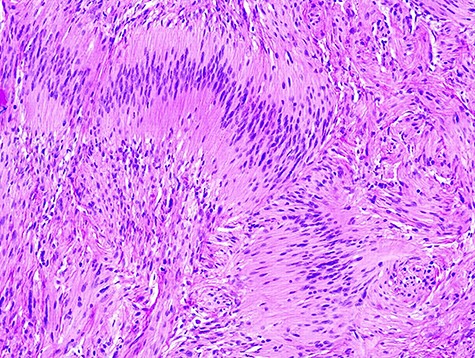
Typical spindle cells of schwannoma with hipo and hyper cellular areas.
With 4 months follow-up, the patient is asymptomatic with a good functional and esthetic result (Fig. 5). She is in a rehabilitation program to improve mouth opening.

DISCUSSION
Parapharyngeal or lateral pharyngeal area is an anatomic virtual space compared to an inverted pyramid located deep in the neck. Its base is the skull base and its top is found in the great horn of hyoid bone. It is bounded anteriorly by the pterygomandibular raphe, posteriorly by the pre-vertebral fascia, medially by the lateral pharyngeal wall and laterally by the deep cervical fascia, the mandible, the parotid gland and the medial pterygoid muscle. It can be divided by the fascia from the styloid process to the tensor veli palatine muscle into two areas: the pre-styloid or anterolateral and post-styloid or post-eromedial compartment. The first compartment contains the following structures: maxillary artery, inferior alveolar nerve, lingual nerve auriculotemporal nerve, adipose tissue and lymph nodes. The second compartment contains the internal carotid artery, jugular vein, cranial nerves from IX to XII, the cervical sympathetic trunk, lymph nodes and fat.
Parapharyngeal space primary tumors are rare, representing less than 0.5% of head and neck tumors [1–3]. As it is a complex anatomic region, it is not surprising that a vast multiplicity of tumors, malignant and benign can be found in this region of the human body. The majority of these tumors are benign (80%) [2, 3, 5]. Near 45% are salivary gland tumors, being the most frequent pleomorphic adenoma [3, 4, 7], followed by neurogenic lesions located mainly in the post-styloid area, as schwannomas or paragangliomas.
Schwannomas, also known as neurilemmomas or neuromas, are rare benign neoplasms derived from nerve sheath of any peripheral, cranial or sympathetic nerve, except olfactory and optic nerve [2]. Schwannomas rarely have a malignant transformation; however, it can occur [2]. The challenge in schwannomas is its proper diagnosis due to its slow growth and almost asymptomatic course leading to unexpected findings in CT scans or MRI.
When facing a high grade of suspicion, complementary radiologic methods are crucial to confirm the diagnosis [6, 7]. CT and MRI are the methods of choice. They can give us a detailed image of the tumor, determine the real dimension and relationship with surrounded structures and help to evaluate the best approach for its removal. CT and MRI can be used as the first choice to complement our investigation; however, MRI has a better image resolution to identify neurovascular structures. On MR imaging, schwannomas have low T1 and high T2 signal intensities being this exam the gold standard in diagnosis.
Treatment of parapharyngeal schwannomas is a challenge as well. The goal is the complete removal of the tumor while preserving all surrounding structures [7]. There are different surgical approaches to remove parapharyngeal tumors such as transcervical, transparotid, transcervical-transparotid, transmandibular or intraoral; however, we must choose that one that best suits the size and the type of mass we are facing [1, 7].
Frequently, the transcervical approach is associated with lip-split incision and mandibulotomy to improve tumor visualization and dissection, known as transmandibular approach [3].
Survival of benign parapharyngeal tumors, including schwannomas, is excellent, rounding 100% when complete removal [1]. Fortunately, when facing a schwannoma in this area, minimal or no post-surgical complications are perceived, except scars and sensory loss.
CONCLUSION
Diagnostic and treatment of parapharyngeal tumors is not a straightforward mission. It is a challenge due to its complex anatomy, very important structures nearby and precarious approachability. Radiological methods, as CT and MRI, are of main importance when studying the tumor and plan surgical removal. Our main goal is the complete removal of the neoplasia and the preservation of the main structures in parapharyngeal space.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



