-
PDF
- Split View
-
Views
-
Cite
Cite
Esraa Kabawe, Sami Kabawe, Rawan Albakour, Majd Alobied, Ahmad Ghazal, Jejunal intussusception in an adult due to multiple lipomas: a rare case report from Syria, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz162, https://doi.org/10.1093/jscr/rjz162
Close - Share Icon Share
Abstract
Intussusception in adulthood is an uncommon medical condition. Multiple lipomas are a very rare cause of intussusception, and the jejunum is the least common location of lipoma. We report an unusual case of a 37-year-old man presented with non-specific symptoms. Computed tomography of the abdomen revealed a proximal jejunal loop distention. Laparoscopy revealed a jejunal intussusception 40 cm distal to treitz ligament. We switched to open surgery after failure of laparoscopic reduction which showed multiple lipomas as the cause of the intussusception. We resected a segment of 35 cm and reanastomosed the bowel. Three days later, the patient was discharged with uneventful recovery.
INTRODUCTION
Intussusception of the bowel is defined as the invagination of a proximal segment of the bowel into the lumen of the adjacent distal segment, thereby causing bowel obstruction. Intussusception in adults is rare, accounting for only 5% of all cases of intussusceptions, and 1–5% of bowel obstructions in adults [1].
Lipomas are benign fatty tumors that can appear in any part of the gastrointestinal tract with the most common location being the colon (64%), followed by the second part of the duodenum (4%) and less than 2% are found in the jejunum [2, 3].
Small lipomas are usually asymptomatic but lesions exceeding 2 cm diameter can cause acute symptoms such as intussusception or hemorrhage [4].
We report a case of small bowel intussusception due to lipomas in the jejunum.
CASE REPORT
A 37-year-old male patient with insignificant surgical history presented to the Emergency Department of the Hospital with vomiting, distension and discomfort of the upper abdomen for 3 days. He had several episodes of hospitalization for the same presentation which were treated conservatively by nasogastric tube. On physical examination, vitals were normal. The upper abdomen was distended, soft and tender with hyperactive bowel sounds. The digital rectal examination was normal. Laboratory tests were unremarkable, except for increased C-reactive protein. Computed tomography of the abdomen revealed a proximal jejunal loop distention (Fig. 1).
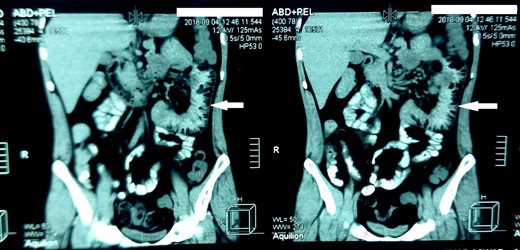
Computed tomography of the abdomen. The arrows indicate dilated proximal loop of the jejunum.
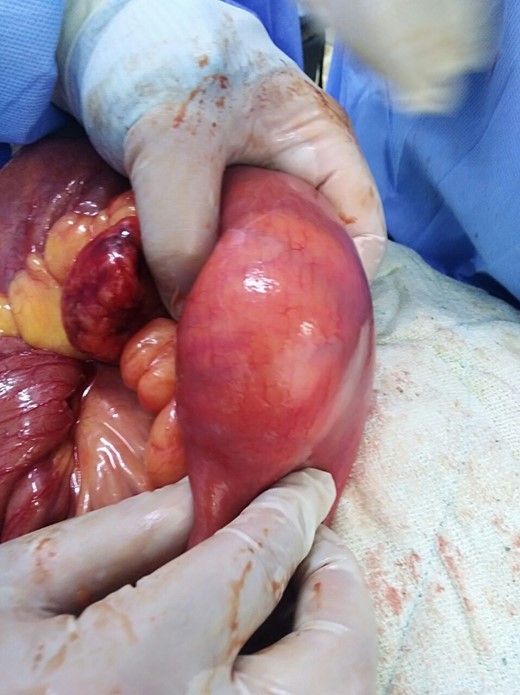
A decision to perform laparoscopic exploration was made, we found jejunal intussusception at approximately 40 cm distal to treitz ligament (Fig. 2). After failure of laparoscopic reduction, we switched to open surgery and we found multiple submucosal and subserosal lipomas ranging from 0.5 to 4.5 cm that caused the intussusception (Figs 3 and 4) and they were associated with ischemic mucosal erosion that is secondary to the intussusception. After the resection of a segment measuring 35 cm containing those lipomas (Fig. 5), we reanastomosed the bowel. We discharged the patient 3 days after the surgery with uneventful recovery.


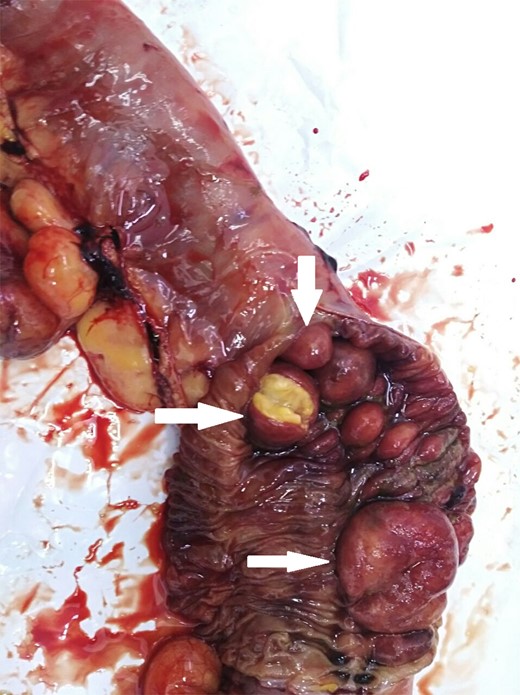
The resected segment of the jejunum. The arrows point to multiple lipomas.
DISCUSSION
Intussusception in adulthood is uncommon, with an incidence of almost 2–3 cases per population of 1 million per year [5], whereas it is the most common cause of intestinal obstruction in infants aged 6–36 months [6].
In adults, only 1% of bowel obstructions are caused by intussusception. Neoplasms are the most common cause of intussusception in adults (60% of causes). These neoplasms are 60% malignant and 40% benign [7].
The majority of benign aetiologies for small bowel intussusception is secondary to polyps of various origins (Peutz-Jeghers, hamartomatous, fibrous, inflammatory), diverticular disease (Meckel’s) and rarely lipomas. Lipomas make up only 1–2% of all gastrointestinal tumors and they most commonly occur in the colon, followed by small bowel and occasionally in the stomach [8].
Among small bowel lipomas, ileal lipomas are the most common and represent 50%, while jejunal lipomas are the least common. They are usually solitary tumors but in only 5% of cases small bowel lipomas could be multiple [8, 9].
We find from above that intussusception in adulthood which is caused by multiple lipomas in the jejunum is a very rare medical condition.
Clinically, intussusception in adults usually has a subacute or chronic onset and the classic pediatric presentation of acute intussusception (a triad of cramping abdominal pain, bloody diarrhea and a palpable tender mass) is rarely seen in adults. Patients commonly present with nonspecific symptoms such as long standing colicky abdominal pain, nausea, vomiting, distention and gastrointestinal bleeding [1, 9].
For the diagnosis, computed tomography (CT) is the radiological modality of choice with a sensitivity ranges from 71.4% to 87.5% while its specificity in adults has been reported to be 100% as verified by the subsequent surgery [5].
Other modalities that may help in the diagnosis are Barium studies and abdominal ultrasound but they have limited sensitivity for diagnosing intussusception when compared to CT scan [8].
The treatment of choice for adult intussusception consists of bowel resection and primary anastomosis [8]. However, controversy remains about whether reduction of the intussusception at operation is necessary [5].
In contrast to intussusception of the colon, where all of the cases should be resected en block without reduction. Some surgeons agree that intussusception of the small bowel should be gently reduced before resection only in patients in whom a definitive benign diagnosis has been made preoperatively and in patients in whom resection may result in short-bowel syndrome. Reduction should not be attempted if there are signs of irreversible bowel ischemia, inflammation, or if a malignancy is being suspected due to the fears of tumor seeding [5, 8].
When patients come with chronic nonspecific symptoms, they pose a challenge for physicians. However, every possibility should be considered with regard to the probability of its incidence until the right diagnosis is found in order to reduce morbidity, physical and emotional distress.
ACKNOWLEDGMENTS
We are grateful to Ms. Nour Ajam for her help in the manuscript editing.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
CONSENT
The patient consent was obtained prior to submission.



