-
PDF
- Split View
-
Views
-
Cite
Cite
Rita Loureiro, Adriano Marques, Júlio Constantino, Carlos Casimiro, Laparoscopic approach for a spontaneous posterior rectus sheath hernia, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz161, https://doi.org/10.1093/jscr/rjz161
Close - Share Icon Share
Abstract
Spontaneous posterior rectus sheath hernia is perhaps one of the rarest hernias described only in a few published cases. We present the case of a small bowel herniation through the posterior rectus sheath in a woman without previous abdominal surgical history, resulting in acute small bowel obstruction who was successfully treated by laparoscopy. This is the first case report of this kind of hernia managed with laparoscopic technique. Although the laparoscopic approach is not considered standard treatment for strangulated hernias, in selected cases, it allows the identification and repair of the defect.
INTRODUCTION
Hernia is an abnormal protrusion of an organ or tissue through a defect in the structure by which it is normally contained [1]. It can be congenital or acquired and is classified according to its anatomical location.
A posterior rectus sheath hernia is a very rare type of abdominal wall hernia, described only in a few published cases [2, 3]. These hernias are considered interparietal because the sac lies between the layers of the abdominal wall [3, 4]. The majority of these hernias are postsurgical or posttraumatic, with limited spontaneous cases being reported in the literature [2].
We present the case of a small bowel obstruction secondary to an incarcerated posterior rectus sheath hernia.
CASE REPORT
A 71-year-old woman presented to emergency department with a three days history of worsening abdominal pain, nausea and vomiting. Past medical history included a vaginal hysterectomy and surgery of the hip. She had no previous history of abdominal surgery and no regular drug history. Physical examination revealed normal vital signs and a distended abdomen with diffuse tenderness but without peritoneal signs.
Blood tests were within normal limits except for an elevated serum creatinine of 1.3 mg/dl and C-reactive protein of 2.4 mg/dl. The abdominal X-rays showed small bowel distension with air fluid levels (Fig. 1). An abdominal computed tomography (CT) scan was performed diagnosing small bowel obstruction secondary to an incarcerated hernia in the left upper abdominal wall. The hernia defect lied through the internal oblique and transversus abdominis muscles aponeurosis with its sac extending posterior to the left rectus abdominis. There weren´t signs of intestinal ischemia (Figs 2 and 3).
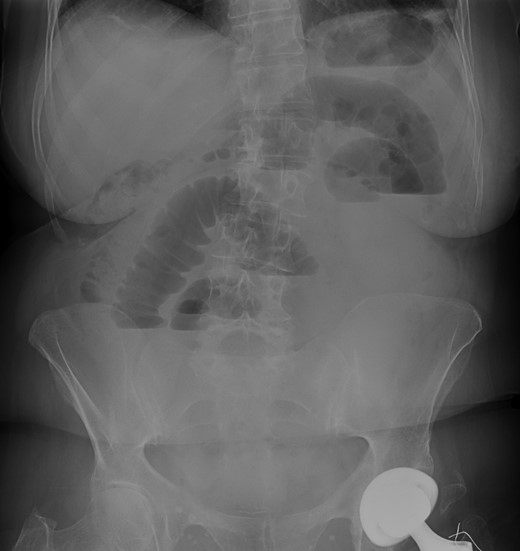
Abdominal X-rays—small bowel distension with air fluid levels.
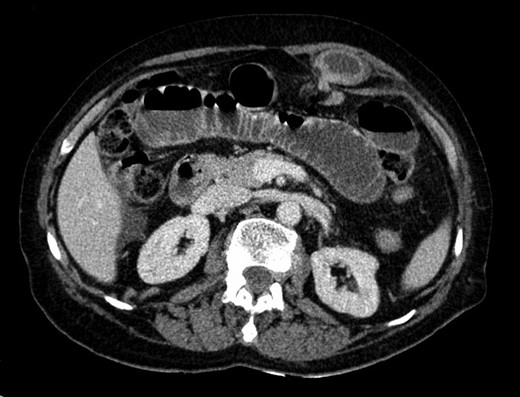
CT scan—axial view of incarcerated hernia with its sac posterior to the left rectus abdominis.

The patient underwent an urgent laparoscopy which showed small bowel herniating through the defect in the left posterior rectus sheath located above the arcuate line (Fig. 4). The hernia was reduced and the defect was repaired laparoscopically with polypropylene/PTFE mesh (Figs 5 and 6). The incarcerated segment of small bowel was edematous with a stenotic and ischemic area and therefore was resected through a small periumbilical incision. The procedure was performed with three incisions (two in rights quadrants and one in umbilical area) (Fig. 7).
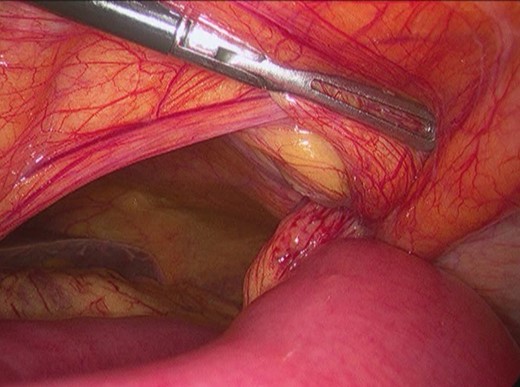
Surgery—intraoperative findings: small bowel incarcerated in the left upper abdominal wall hernia.


Surgery—laparoscopic mesh repair with polypropylene/PTFE mesh.
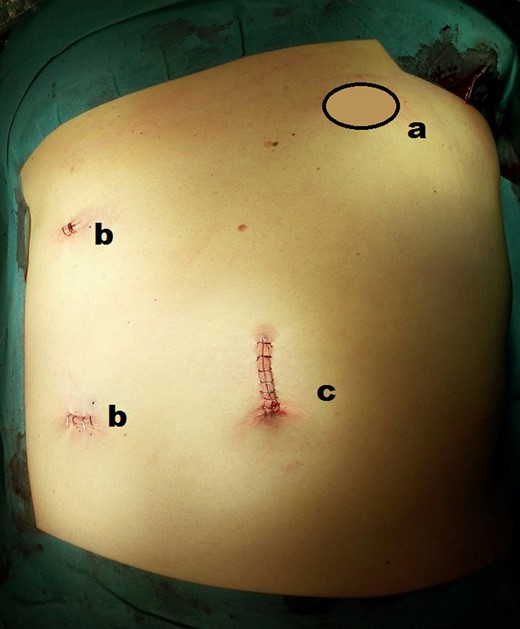
Final abdominal view—(a) hernia location; (b) local of two 5 mm ports; (c) local of 10 mm port and subsequent incision to preform small bowel resection.
The patient had an uneventful postoperative course and was discharged three days after surgery. She was seen 2 months after the surgery and was free of complaints.
DISCUSSION
Spontaneous posterior rectus sheath hernias were first documented in 1937 and there are only 10 cases published in the literature [2, 3, 5]. They belong to the group of interparietal hernias in which the hernia sac lies between the layers of the abdominal wall [4].
Most of interparietal hernias were identified in the inguinal region and are classified as preperitoneal, interstitial and superficial according to the anatomical location of the sac [6].
Posterior rectus sheath hernia belong to the interstitial group because the sac lies between the muscles layers of the abdominal wall and does not exit into the subcutaneous tissue [7].
The rectus abdominis muscle is enclosed within the rectus sheath which is formed by the aponeuroses of the lateral abdominal muscles [3]. Its anterior layer consists of the external oblique aponeurosis supplemented by the anterior aponeurotic layer of the internal oblique aponeurosis, whereas its posterior layer is formed by the aponeurosis of the transversus abdominis muscle and the posterior aponeurotic layer of the internal oblique aponeurosis up to the level of the arcuate line. However, below the arcuate line, all three aponeuroses pass anterior to the rectus abdominis muscle [7].
Despite the fact that the most vulnerable part is below the arcuate line, the majority of the reported cases, including ours, occurred in the supraumbilical region [1–3]. The theory behind the formation of these hernias is that they appear at the sites of reduced resistance such as where the neurovascular structures pass through the aponeurosis [4, 7].
In the published literature, as well as in our case, most of spontaneous posterior rectus sheath hernias were diagnosed only when presenting with complication such as small bowel obstruction [2]. We assume that asymptomatic hernias are not found because the sac lies between the abdominal wall layers and there is no bulging.
When they cause symptoms, these are frequently nonspecific (pain, distension, and vomiting) and the hernia is not identified by the physical examination [2, 5]. In the majority of the reported cases, the hernia was diagnosed by CT scan [2, 3]. This is the best diagnostic modality to identify the cause of small bowel obstruction and provides good anatomic detail of the abdominal wall which allows to detect hernias that aren’t clinically evident and their complications.
Laparoscopy may be a useful tool in selected cases of abdominal wall hernias presenting with small bowel obstruction providing the ability to diagnose and to repair these hernias. In our case, we performed a laparoscopy that confirmed the intestinal entrapment and enabled us to do a minimally invasive repair.
Mesh repair provides a more durable long-term result with fewer recurrences, particularly when the hernia defect is large, but it’s an option only when there’s no overt contamination. [2, 3].
To our knowledge there are no other cases describing a laparoscopic management for a posterior rectus sheath hernia presenting as small bowel obstruction [2]. This approach enabled us to correctly identify the hernia site and safely perform the bowel reduction and the mesh repair.
In conclusion, we describe a very unusual case of a posterior rectus sheath hernia presenting as a small bowel obstruction. Prompt diagnosis of these cases is fundamental and laparoscopic surgery is a valuable option for their treatment.
CONFLICT OF INTEREST STATEMENT
None declared.



