-
PDF
- Split View
-
Views
-
Cite
Cite
Ioannis Delniotis, Benedikt Leidinger, A 10-year follow-up of asymptomatic Charcot hip joints caused by CIPA syndrome (congenital insensitivity to pain with anhidrosis) with failure of any surgical reconstructive treatment, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz154, https://doi.org/10.1093/jscr/rjz154
Close - Share Icon Share
Abstract
Congenital insensitivity to pain with anhidrosis (CIPA) is a rare genetic disorder. Patients with CIPA lack among other things the protective sensation of pain. Orthopaedic manifestations are fractures, infections and hip joint dislocation. We report a 10-year follow-up of late developing hip dysplasia with CIPA and the result of several reconstructive surgical procedures. The final outcome was asymptomatic Charcot hip joints with superior migration and dislocation of both hips without pain. In conformance with the literature standard operative techniques in these rare cases usually seem to fail. A multidisciplinary conservative approach with close observation and activity modification is the proposed treatment of choice.
INTRODUCTION
Congenital insensitivity to pain with anhidrosis (CIPA) is a rare, genetic disease that is mainly characterized by lack of pain sensation and inability to sweat [1]. As a result, these patients are susceptible to multiple and recurrent injuries, bone fractures and joint dislocations [2]. Severe complications have been reported in joint preserving surgery of the hip in these patients [3–6]. We describe a case-report of a patient with CIPA and development of a bilateral progressive and destructive hip dysplasia despite reconstructive surgical intervention with a 10-year follow-up. To our knowledge, our study is the first report providing such a long term observation of a patient suffering from CIPA and destructive hip dysplasia.
CASE PRESENTATION
Ten years ago, a 12-year-old male presented to our clinic complaining about limping and massive swelling of the left hip. Figure 1 shows the initial X-ray and the 3D reconstruction of the left hip at first presentation when the femoral head, had already destroyed the lateral edge of the acetabulum like a mortar. Severe pain episodes have apparently not been noticed and a former hip dysplasia was not known. A brief clinical history revealed that the patient presented repeated episodes of finger biting and fevers from 2 to 8 years old. The intelligence level of the patient was at an average. The patient was admitted to a paediatric neurologist and a genetic test. A mutation of the NTRK1 gene was found and the diagnosis of CIPA was established. The right hip initially appeared to be normal and the patient was walking, therefore surgical reconstruction for the left hip was proposed due to massive swelling, inability of normal walking and significant limb length discrepancy. A Tönnis/Kalchschmidt triple pelvic osteotomy with open reduction and a shortening varus derotation osteotomy (VDRO) of the femur was performed (Fig. 2A–B). After 3 months the patient was walking again but another 3 months later the hip dislocated again without severe pain. Although the femoral head was already damaged the hip joint was reconstructed again by open reduction, capsular reconstruction with suture anchors and a trevira tube and a movable external fixator was used to temporary stabilize the joint (Fig. 3). The right hip at this time was still intact and was protected with a pneumatic orthotic device. A few months later in 2009, despite all surgeries, the left hip had entirely lost congruency and the right hip developed subluxation despite conservative treatment (Fig. 4). The patient was still walking so the decision to reconstruct the right hip with open reduction, capsular augmentation with a trevira tube, a triple pelvic osteotomy and VDRO was made (Fig. 5). Few months later this reconstruction failed as well and the hip dislocated without severe pain (Fig. 6).
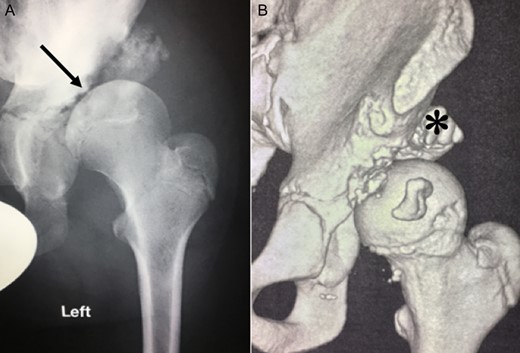
(A + B): (2008) (A) X-ray of the left hip demonstrating subluxation of the femoral head which is destroying the edge of the acetabulum (arrow) like a mortar. (B) 3-D reconstruction of the hip showing bony debris of the acetabulum edge forming a secondary acetabulum (asterisk) trying to cover the femoral head.
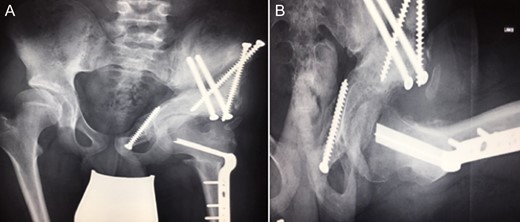
(A + B): (2008) (A) Hip reconstruction with open reduction, Tönnis triple pelvic osteotomy and shortening rotational varus osteotomy of the left femur demonstrating correct deep reposition in ap view. (B) Lauenstein view shows that the acetabular congruency over the femoral head is restored.

(2008) Despite reconstruction the femoral head subluxated and rapidly lost congruency. An open reduction and capsular reconstruction with trevira tube, removal of the femoral plate and temporary fixation with an external fixator with movable hip mechanism for flexion of the joint (Orthofix MonoRail) was performed.

(2009) Despite conservative treatment the right hip subluxates. There is new bone formation at the proximal os ileum (asterisk) without trauma. The acetabulum is still congruent and decision was made to restore the hip joint by surgery.
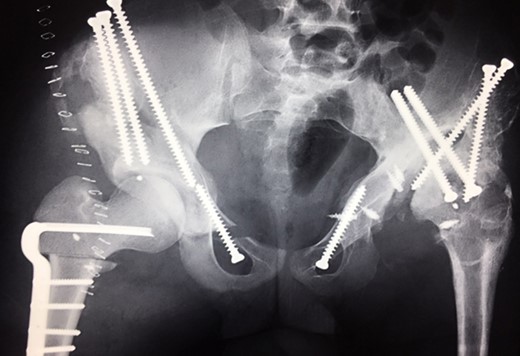
(2009) Operative reconstruction of the right hip with open reduction, capsular reconstruction with trevira tube augmentation, triple osteotomy and DVO of the proximal femur to prevent destructive degeneration was performed.

(2010) Hip dislocation of the right side despite reconstruction.
At this stage patient’s walking ability was already limited due to muscle weakness and rubbing in the hip joints, so we recommended no further walking and weight bearing. Further follow-up at 5 years (Fig. 7) and 10 years (Fig. 8A) until today showed radiologically complete absorption of the left femoral head and the right hip continuously moving cranially creating a false acetabulum and a flattened femoral head. At final follow up the patient was in a wheel chair but able to bend both hips up to 110 degrees without noticeable pain, he could stand up with help for a short time and showed a massive Charcot joint with effusion (Fig. 8B) of the right hip without further clinical implications.

(2013) Further destruction of any bony congruency at the left side, dislocation on the right side.
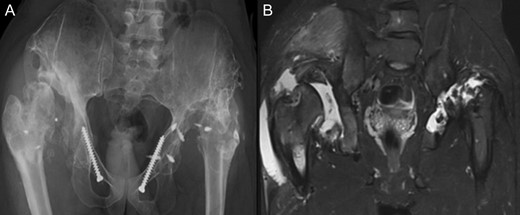
(A + B): (2019) (A) x ray of the pelvis after a 10 year follow up. The right head further migrated und subluxated and femoral head necrosis is visible, new bone formation at the ileum stabilizing the joint. At the left side high dislocation of the hip with fully necrosis of the head and ankylosis of the hip joint. (B) MRI showing hip effusion around the joint which is painless.
DISCUSSION
The insensitivity to pain is probably the most dangerous characteristic of this disease. Bruises, cuts, fractures, dislocations and burns can appear [6]. Zhang et al. report that 59 out of 91 CIPA patients (65%) suffered from fractures and 27/91 patients (30%) had joint dislocations, mainly of the hip. Most of these patients (29%) developed Charcot joints [6].
Whereas hip problems in elderly patients with CIPA caused by fracture and avascular necrosis show successful short term results treated by joint arthroplasty [7, 8], hip dysplasia and dislocation seem to develop late. Ordinary joint preserving strategies with different techniques although well performed fail as reported by Szöke et al., Bar-On et al., Wang et al. and Zhang et al. [3–6]. Bar-On E. et al. reviewed 13 patients with CIPA and describe three clinical subtypes of the disease with type C predestinated for joint dislocation [4].
Our patient initially presented with massive joint effusion after development of late hip dysplasia which also could not be treated successfully by surgery regardless which technique was applied. It ended up with severe destruction of both hips. Reviewing the literature, it seems that the recommendation for hip dislocation in patients with CIPA syndrome is conservative treatment and no surgical intervention [3–6]. Early immobilization might prevent or at least slow down the development of destructive hip dysplasia [4]. If Charcot joints develop, these are mostly asymptomatic and do not require specific treatment even after years.
The other main characteristic of CIPA patients is anhidrosis [9]. The inability to sweat can lead to recurrent fevers and this clinical sign can be one of the first clinical characteristics of CIPA, appearing also in infancy [9].
Indo Y. states that the impaired pain sensation seems to be the reason that specifically the hip joints (weight bearing joints) are so commonly affected. The reason for this seems to be the loss of intrinsic joint stabilization mechanisms [10].
CONCLUSION
Joint preserving surgery for late developing hip dysplasia in patients with CIPA syndrome seems to be ineffective no matter what techniques are applied. Orthopaedic surgeons should be aware of this rare condition. The best treatment for these patients is conservative and supportive with activity modification. In the end, the patients end up with massively dislocated Charcot hip joints and joint effusion. The clinical severity of this condition is less difficult than expected and the patients are able to tolerate this condition due to their lack of pain sensitivity even after years.
CONFLICT OF INTERESTS
There are no conflicts of interest associated with this publication and there has been no financial support for this work that could have influenced its outcome.
FUNDING
The authors received no financial support for the research, authorship and/or publication of this article.
INFORMED CONSENT
Informed consent was obtained from the patient for his anonymized information to be published in this article.



