-
PDF
- Split View
-
Views
-
Cite
Cite
Waleed Mohammed Alshehri, Suhaib Khalid Alothmani, Abdullah Mohammed Alshamrani, Rahaf ibrahim Almadhari, Adel Saad Alqahtani, D Alrasheedi Saud, Internal jugular vein aneurysm: a case report, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz159, https://doi.org/10.1093/jscr/rjz159
Close - Share Icon Share
Abstract
Venous aneurysms rarely present as a painless mass; they are usually symptomatic and present with pain, swelling, and sometimes, embolism. We present a 41-year-old man who presented with a painless swelling involving the right side of the neck. Examination of the neck revealed a soft, compressible, non-pulsatile and non-tender swelling above the right sternoclavicular joint. Doppler ultrasound showed a well-defined compressible cystic lesion measuring 4.2 × 1.9 cm causing indentation of the right sternocleidomastoid muscle. Further imaging studies confirmed the diagnosis of an aneurysmal dilation in the right internal jugular vein. An excisional biopsy of the aneurysm was performed using a longitudinal incision in the skin at the anterior border of the right sternocleidomastoid muscle and excisional venotomy was performed. Histopathological examination showed a cystic structure containing organizing blood clots surrounded by a thick fibrous wall. A follow-up neck ultrasound performed postoperative showed a patent internal jugular vein.
INTRODUCTION
An aneurysm is a localized dilatation of the vessel wall that involves all its layers. Venous aneurysms rarely present as a painless mass; they are usually symptomatic and present with pain, swelling, and sometimes, embolism.
The pathology is benign, although serious complications such as a rupturing of the aneurysm, pulmonary embolism, and thrombosis have been reported in some patients [1, 2]. Although the mechanism underlying the pathology has not been established, it has been suggested that structural changes within the blood vessel occur due to an increase in matrix metalloproteinases [3]. Its age-specific incidence has not been reported, but any age group can be affected.
Here we present the case of a 41-year-old man, who presented with a painless swelling involving the right side of the neck. An ultrasound, computed tomography (CT) scan, and magnetic resonance imaging (MRI) confirmed the diagnosis as internal jugular vein aneurysm.
CASE PRESENTATION
A 41-year-old Saudi man living in Riyadh presented to the outpatient department of our hospital with the chief complaint of a painless mass in the right side of the neck. The mass was discovered accidentally by the patient himself 6 years earlier. It had been stable in size until 2 months ago, when it started growing slowly, becoming cosmetically embarrassing for the patient. The patient did not have any significant surgical or medical history, nor was there any history of head or neck trauma. However, he had a history of liposuction for gynecomastia.
An examination of the neck confirmed a soft, compressible, non-pulsatile, and non-tender swelling above the right sternoclavicular joint. A Valsalva maneuver caused enlargement of the mass.
A Doppler ultrasound showed a well-defined, compressible, cystic lesion measuring 4.2 × 1.9 cm, causing an indentation of the right sternocleidomastoid muscle. It contained a venous pattern of flow with communication between itself and the internal jugular vein (Fig. 1).

A Doppler ultrasound showing a well-defined, compressible, cystic lesion measuring 4.2 × 1.9 cm, causing an indentation of the right sternocleidomastoid muscle. The mass contained a venous pattern of flow with communication between itself and the internal jugular vein.
A CT scan exam with contrast was performed, which confirmed the presence of dilatation measuring 31.6 × 42.31 mm on cross section in the internal jugular vein (right side) in the lower part of the neck (Fig. 2A). Magnetic resonance venography (MRV) was ordered, which further confirmed the diagnosis of an aneurysmal dilatation in the right internal jugular vein (Fig. 2 B and C).
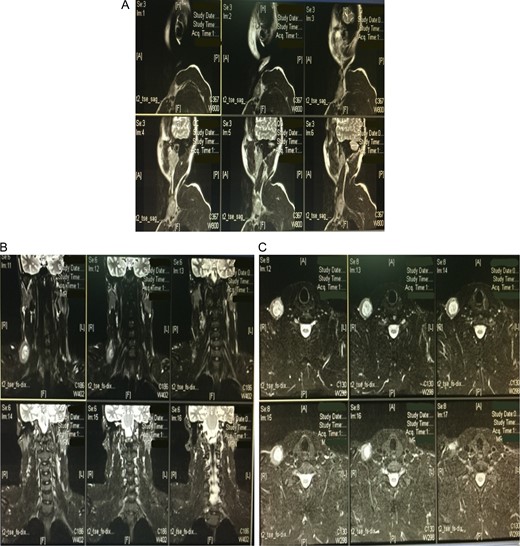
A computed tomography scan with contrast showing a dilatation in the internal jugular vein (right side) in the lower part of the neck measuring 31.6 × 42.31 mm on the cross section (A). Magnetic resonance venography further confirmed the diagnosis of an aneurysmal dilatation in the right internal jugular vein (B and C).
An excisional biopsy of the aneurysm was performed using a longitudinal incision in the skin at the level of the anterior border of the right sternomastoid muscle (Fig. 3). An excisional venotomy was also performed, and a whole aneurysmal wall excision done. Finally, the internal jugular vein was closed using a 5.0 Proline suture. Hemostasis was accomplished, and the specimen was sent for histopathological examination. A histopathological examination of the mass showed a cystic structure containing organizing blood clots surrounded by a thick fibrous wall, suggestive of an organizing thrombosis (Fig. 4).
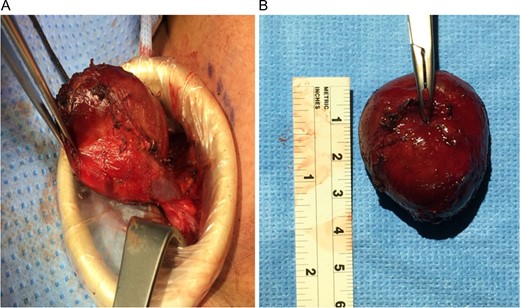
An intraoperative image showing the aneurysmal mass attached to the right internal jugular vein (A). An intraoperative image taken after excisional venotomy and whole aneurysmal wall excision were performed (B).
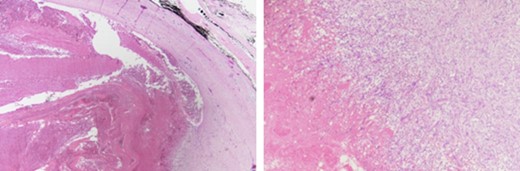
A histopathological examination of the mass showed a cystic structure containing organizing blood clots surrounded by a thick fibrous wall, suggestive of an organizing thrombosis.
The patient did well postoperatively, and he was discharged one day later. According to the patient, his condition improved, and he could function well again. A follow-up neck ultrasound performed one month postoperative showed that the previously noted cystic lesion was no longer visible and the internal jugular vein was patent.
DISCUSSION
Primary aneurysms in the venous system are very rare; only 311 cases had been reported by the end of 1992 [4]. The first case was reported in a five-month-old child in 1928 by Sommer et al. [5], and the aneurysm was described as a congenital cyst in the superior vena caval system [6]. In 1984, Danis [7] described three cases in which an excisional biopsy was performed; histopathological findings revealed a focal thickening of the intimal layer, an increase in the amount of connective tissue, and an increase in the endothelial cells in comparison to the veins with non-aneurysmal components. Schatz et al. [8] described two major pathological findings in patients with venous aneurysms, the first being reduced smooth muscle cells, and the second, an increase in the fibrous connective tissue.
Aneurysm of the neck veins is a self-limiting and benign condition, and complications such as thrombophlebitis, embolism, or thrombosis are rarely reported [1, 2]. Treatment options for aneurysms of the internal jugular vein include surgical resection or conservative management with a follow-up. Surgical resection is performed for symptomatic aneurysms and for cosmetic reasons while conservative management is preferred for asymptomatic cases [9]. Karapolat et al. [10] suggested that surgical treatment should be considered, especially given the risk of thrombosis, which could lead to pulmonary embolism or rupture.
The most common presentation of a patient with a venous aneurysm is a soft, compressible swelling at the level of the vein axis [9]. Non-invasive techniques for imaging and diagnosis include Doppler ultrasound, multidetector CT scan, angiography, and MRV [3]. Following an aneurysmal excision, either ligation of the vein involved or bypassing it using a graft is performed, and treatment depends on whether it is feasible to sacrifice the vessel. In general, the approach is mainly based on the size and location of the aneurysm. Irrespective of the approach, it is imperative that the clinician confirm contralateral patency prior to surgery to prevent cerebral edema [5]. A previous report [9], described the cases of two patients who underwent unilateral ligation of bilateral lesions and developed cerebral swelling three days later. However, no study has compared long-term outcomes in patients who had different treatment strategies for internal jugular vein aneurysm.
In conclusion, an internal jugular vein aneurysm is a benign condition that can be managed conservatively. Surgical resection may be indicated for cosmetic reasons or symptomatic cases. The procedure is well tolerated and follow up imaging is necessary to confirm the patency of the internal jugular vein.
CONFLICT OF INTEREST STATEMENT
The authors declare no potential conflict of interests with respect to the research, authorship, and/or publication of this article.
REFERENCES
- neck
- edema
- aneurysm
- doppler ultrasound
- cysts
- dilatation, pathologic
- follow-up
- pain
- phlebotomy
- sternoclavicular joint
- diagnosis
- diagnostic imaging
- skin
- thrombus
- embolism
- excisional biopsy
- internal jugular vein
- sternocleidomastoid muscle
- neck ultrasonography
- patents
- right internal jugular vein
- examination of neck
- histopathology tests



