-
PDF
- Split View
-
Views
-
Cite
Cite
Yutaka Kojima, Kazuhiro Sakamoto, Yuichi Tomiki, Rina Takahashi, Ryoichi Tsukamoto, Toshiaki Hagiwara, Kunihiko Nagakari, Cases of low anterior resection and ileostomy for rectal cancer that required more than 18 months for stoma closure, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz153, https://doi.org/10.1093/jscr/rjz153
Close - Share Icon Share
Abstract
Laparoscopic surgery is performed worldwide, even for cases of rectal cancer close to the anus, and advances in surgical instruments and techniques have increased the number of cases for which anastomosis can be performed, even those cases for which abdominoperineal resection was performed previously. Consequently, as a measure to avoid complications in the event of suture failure after surgery, the number of cases of establishing diverting stoma has also increased. Diverting ostomy may require a closure operation earlier than planned due to colostomy complications, cases requiring a long period of time until closure due to postoperative complications, and cases in which closure operation cannot be performed. Herein, we report cases that took more than 36 months to allow closure of the diverting stoma.
INTRODUCTION
With the spread of laparoscopic and robot-assisted surgery and improvements of surgical equipment and techniques, anastomosis has become possible for rectal cancer near the anal verge. Concomitantly, the incidence of anastomotic leakage has also increased and diverting stomas have often been created. The diverting stoma is usually closed around 8–12 weeks after surgery [1], but it may take a long time to close due to postoperative complications. One concern is that it could take a long time until stoma closure, which may cause dysfunction of the intestine and anal dysfunction, and increase the time to recovery. We report two cases of ileostomy closure more than 18 months after the first operation.
CASE REPORT
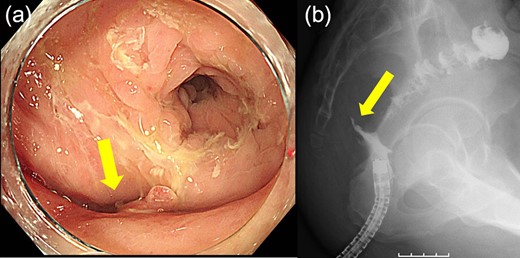
Case 1 was a 71-year-old man with a BMI of 29.7 kg/m2. Laparoscopic low anterior resection (LAR) and ileostomy was performed for rectal cancer in 2017 years. Postoperative fever and lower abdominal pain were noted, and colonoscopy was performed, and anastomotic leakage was noted with a correction of about 1/2 around the 6 o’clock direction of the anastomotic region, and fistula and formation of a large abscess cavity. After identification (Fig. 1), a tube was inserted for drainage and conservative treatment was performed. The patient was discharged on POD 46. Four months after the operation, marked improvement in the abscess cavity was noted but still remained (Fig. 2a and b). Anastomotic leakage was almost improved by colonoscopy at 17 months after surgery, but at the preference of the patient we performed colostomy 22 months after surgery (Fig. 3). It took a long time to improve intestinal movement of the colon because the large intestinal tract had not been used for a long time, and conservative treatment was performed using a nasogastric tube for paralytic ileus. Diet was initiated 7 days after surgery, and the patient was discharged from the hospital 14 days after surgery. The Wexner score [2] was 19 points one month after closure, 17 points 3 months after the operation and 16 points after 6 months after the operation, and severe anal dysfunction was observed, but gradually improved.
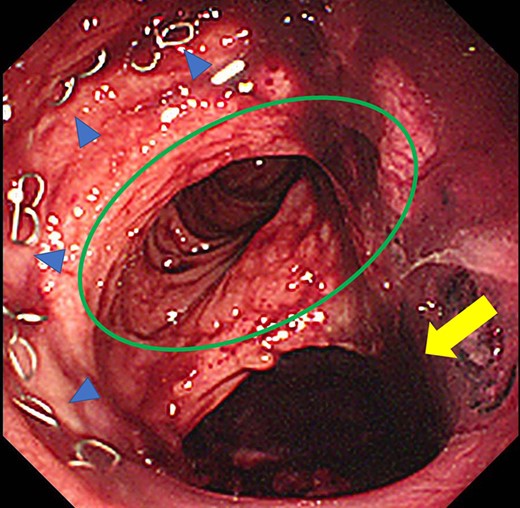
Colonoscopy revealed a true lumen (circle), an anastomotic site (triangle) and a cavity due to suture failure (arrow).
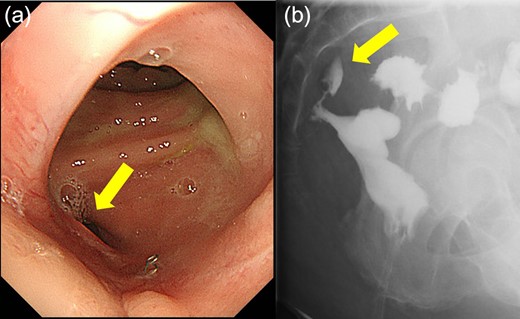
(a) Colonoscopy shows a fistula (arrow). (b) Enema examination shows a cavity (arrow) leading from the fistula.
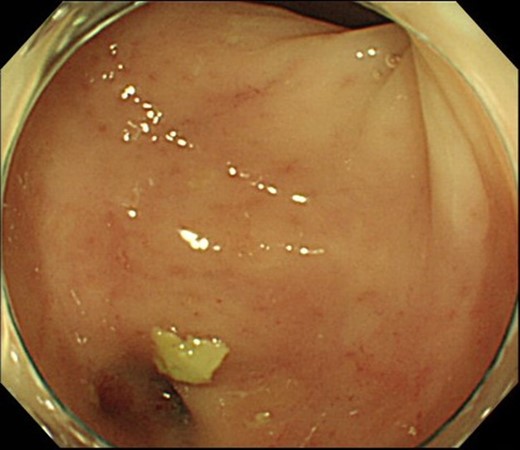
Colonoscopy shows that the suture failure has improved with only a slight depression.
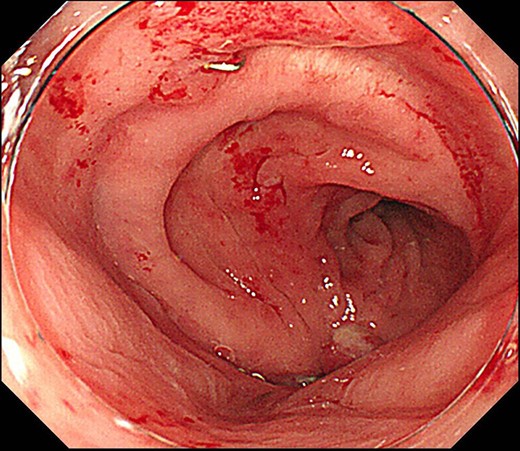
Case 2 was a 58-year-old man with a BMI of 30.3 kg/m2. Robot-assisted LAR and ileostomy was performed for lower rectal cancer over the past 2017 years, and a 1/2 circumferential fistula around the 6 o’clock direction was recognized on postoperative colonoscopy (Fig. 4). The patient was diagnosed as having a grade A anastomotic leakage without symptom because of the anastomotic leakage. He was discharged on POD 26 and was followed up on an outpatient basis. Contrast imaging performed simultaneously with endoscopic examination 6 months after the operation showed remarkable improvement of the abscess cavity, but it still remained (Fig. 5a and b). The anastomotic leakage improved 11 months after surgery (Fig. 6), but a polyp was found on the anal side 2 cm from the anastomotic site and was resected. Adenocarcinoma, pTX, ly0, v0, pHMX, and pVMX were diagnosed. The tumor was followed up because the depth of penetration, the deep stump, and the horizontal stump remained unknown (Fig. 7). Regarding the polypectomy site, no abnormality was found in the examination 8 months after resection of the polyp. Therefore, ileostomy closure was performed 18 months after the first operation (Fig. 8). Postoperatively, it took some time to improve the intestinal movement with paralytic ileus, but the patient was discharged 18 days after surgery. The Wexner score one month after closure was 18 points and still showed high anal dysfunction but the patient was under observation at the outpatient department.
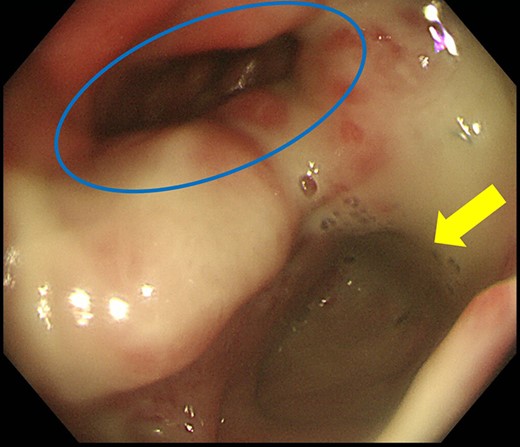
Colonoscopy shows a true lumen (circle) and an abscess cavity (arrow) with drainage of pus.
(a) Endoscopic examination shows improvement of the suture failure and fistula formation (arrows). (b) Enema examination shows fistula (arrow).
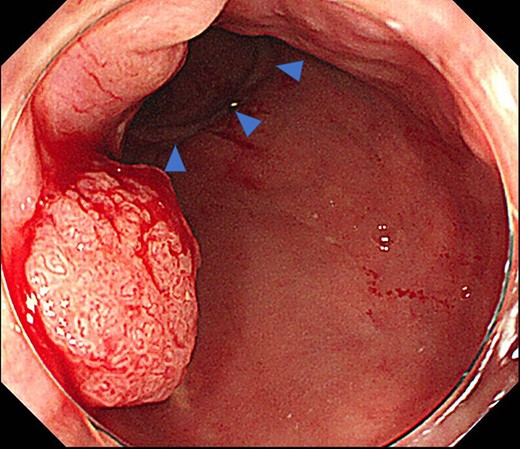
Colonoscopy reveals a polyp on the anal side, about 2 cm from the anastomotic site (triangle).
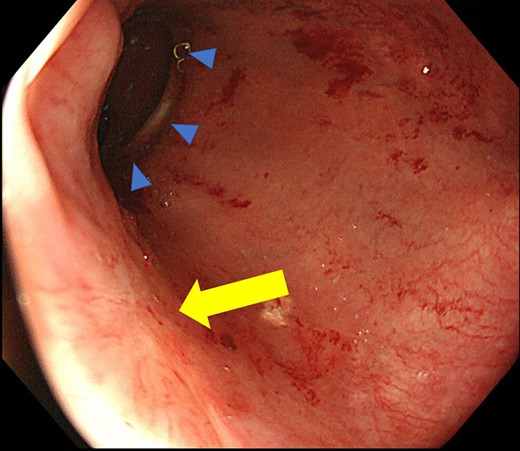
Colonoscopy shows a scar after polypectomy, but no sign of recurrence, and an anastomotic site (triangle).
DISCUSSION
LAR with ileostomy has certain advantages over LAR without ileostomy in terms of anastomotic leakage, postoperative ileus, resumption of diet, wound infection, small bowel obstruction, mortality and recurrence [3]. It has become possible to perform this procedure, and the opportunity to construct a diverting stoma has increased accordingly. The time to close the diverting stoma has been reported to be 6-12 weeks [4–6]. However, according to Waterland et al., only 75% of cases were closed, the median time to surgery was 6 months (1–42 months) and 50% of cases were closed after 6 months or more. In addition, in 35% of cases, adjuvant chemotherapy is the second most common complication after adjuvant surgery, as a cause for delaying closure, and 14% of cases were due to anastomotic leakage [1]. Even in one of our cases, as there was a large abscess formation due to anastomotic leakage, we waited for improvement prior to performing closure and the time from the first surgery became prolonged.
In addition, it has also been reported that the anastomotic leakage rate was significantly higher in cases in which the anus could not be returned compared with those cases in which it was able to return [1]. Anastomotic leakage was considered to greatly affect the closing of the diverting stoma and its timing.
It is said that the time taken to close the diverting stoma affects anal function.
It has been reported that closure of the colostomy within 3 months results in better anal function [7]; thus, it is important to aim to reverse the diverting stoma as soon as possible. However, there are also cases in which the time to reverse is delayed due to postoperative complications, such as leakage and cases in which adjuvant chemotherapy should be prioritized after surgery. In our cases, the improvement was time-consuming due to leakage, and the diverting stomas were closed 18 months or more after the first operation. Thus, it took a long time to improve the postoperative intestinal movement and anal function. The reduction of the treatment period by End-SPONGE® (B.Braun, Austria, GmbH) in cases of abscess formation due to anastomotic leakage has also been reported [8], and it is thought that it is necessary to accumulate a greater number of measurements and cases to reduce postoperative complications in the future.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES



