-
PDF
- Split View
-
Views
-
Cite
Cite
Christopher L Kalmar, Tananchai A Lucktong, Laparoscopic enteropexy for intussusception at Roux-en-Y anastomosis, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz152, https://doi.org/10.1093/jscr/rjz152
Close - Share Icon Share
Abstract
Roux-en-Y gastric bypass (RYGB) is the most commonly performed bariatric procedure in the world. Jejunojenual intussusception after RYGB is a rare but potentially serious complication. Timely radiographic recognition and surgical therapy with laparoscopic enteropexy of all limbs of the enteroenteric anastomosis in our experience allows same-day management with return to work and activities of daily living without recurrence of intussusception.
INTRODUCTION
Roux-en-Y gastric bypass (RYGB) is the most commonly performed bariatric procedure in the world, with 210,874 procedures performed annually [1]. Jejunojenual intussusception after RYGB is a rare but potentially serious complication, with possibility of ischemia and perforation if unrecognized. This diagnosis has the potential to remain unrecognized due to its nonspecific physical exam findings, nonspecific laboratory results, and possible negative imaging studies.
CASE REPORT
A 47-year-old female presented seven years after RYGB complaining of 4-month history of intermittent abdominal pain, abdominal distention, and belching. Eventual workup included CT scan (Fig. 1) with intravenous and oral contrast demonstrating retrograde intussusception of the common limb into the enteroenteric anastomosis.
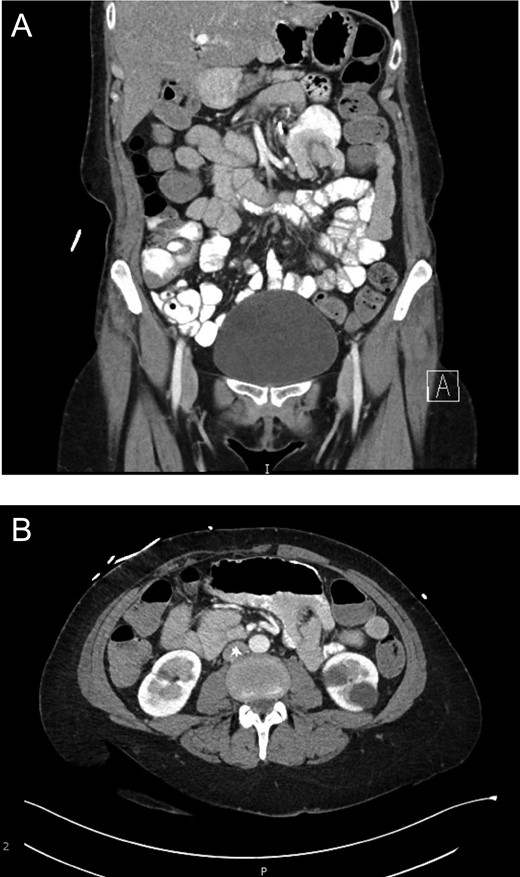
(a) Evidence of intussusception on CT scan (Coronal View). Demonstration of intussusception at the Roux-en-Y enteroenteric anastomosis. (b) Evidence of intussusception on CT scan (Transverse View). Demonstration of intussusception at the Roux-en-Y enteroenteric anastomosis.
Surgical technique
Laparoscopic survey revealed an ante-gastric retrocolic Roux limb. There was no internal hernia at the mesocolon. There was no Peterson’s defect. The enteroenterostomy was dilated. There was no intussusception at the time of exploration; however, the distalmost end of the Roux limb was easily invaginated into the enteroenterostomy with the lead point at the anastomosis. (Fig. 2) On the opposite side of the enteroenterostomy, the common channel limb could likewise easily be invaginated into the enteroenterostomy. There was no evidence of necrosis.
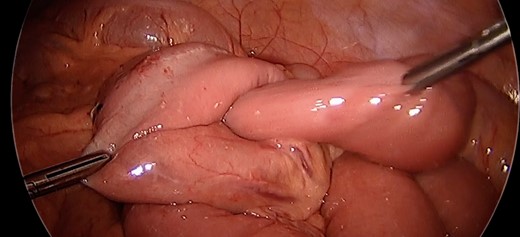
Intussusception. Surgeon manually demonstrating the propensity of the common limb to intussuscept into the anastomosis.
Given the propensity of the distal Roux limb to intussuscept into the enteroenterostomy, enteropexy was performed to eliminate its travel past the anastomosis. The distalmost aspect of the Roux limb was sutured with two pieces of running 3-0 silk to the end of the staple line on the biliopancreatic limb. Two additional sutures were placed slightly more upstream anchoring the roux limb to the mesentery of the transverse colon. An additional 3-0 silk suture was placed on the opposite side of the distal Roux limb anchoring it to the nearby mesenteric root. (Fig. 3) A 3–0 silk suture was placed to fix the common channel to the biliopancreatic limb to similarly limit the risk for intussusception of that limb. After this procedure, the small bowel was immobilized such that there was no longer predisposition for intussusception at the Roux-en-Y enteroenteric anastomosis (Fig. 4).
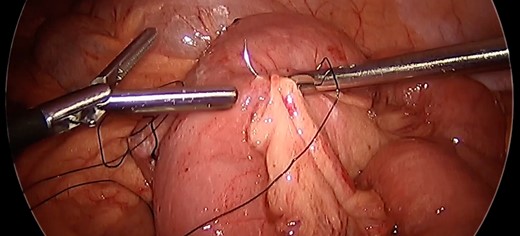
Anchoring bowel to mesenteric root. Nonabsorbable polyfilament suture placement between bowel and nearby mesenteric root limiting bowel mobility toward the anastomotic junction to prevent intussusception.
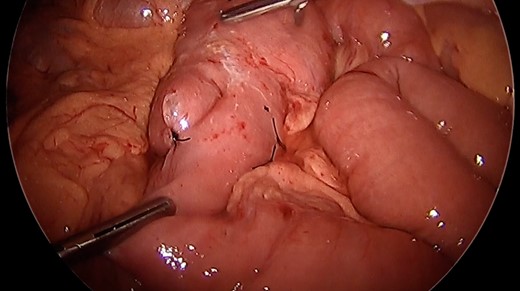
After enteropexy. Demonstration of nonabsorbable suture placement for enteropexy and subsequent inability to intussuscept the common limb into the enteroenteric anastomosis.
Postoperative outcome
The patient tolerated the procedure well and was stable for discharge four hours postoperatively. Follow-up clinic encounter 2 weeks later was significant for left abdominal wall pain prompting CT scan, which remained negative for recurrent intussusception. Pain was distant from our operative site and attributed to nerve impingement secondary to surgical clips placed during previous abdominoplasty. The patient remains without nausea or other sequelae of intussusception two years postoperatively.
DISCUSSION
Jejunojejunal intussusception is a rare but potentially serious complication after RYGB. Estimated incidence of jejunjejunal intussusception is 0.1–1.2% and occurs at a median interval of 36–52 months after the gastric bypass procedure [2, 3]. The classic triad of intussusception (abdominal pain, bloody stools, palpable mass) is only present in 9.8% of adult cases, and is likewise rarely seen with intussusception after RYGB [4, 5]. Nonspecific symptoms, benign physical exam, and nonspecific laboratory results make this diagnosis elusive and necessitate radiographic imaging to achieve the diagnosis. CT with intravenous and oral contrast may demonstrate the classic target sign of intussusception, dilated small bowel, wall thickening, and occasionally vascular compromise. However, 43% of patients with preoperative CT evidence of jejunojejunal intussusception do not have evidence of jejunojejunal intussusception at operative exploration [2]. Due to this dynamic and intermittent process, physicians should remain open to this diagnosis and consider repeated imaging studies if initial scans are negative for intussusception if clinical index of suspicion remains high.
Small bowel intussusception traditionally occurring in adults is due to a pathologic lead point. Although many indicate the staple or suture line to function as a lead point, current thinking implicates abnormal small bowel motility as the culprit predisposing patients to intussusception after RYGB. The duodenum acts as the pacemaker of small bowel motility, but becomes separated from the remainder of the small bowel due to transection of the jejunum to create the Roux limb. Without the presence of the natural pacemaker, ectopic pacemaker potentials arise within the Roux limb. Ectopic pacemaker potentials generate abnormal reverse propagation [6]. This creates Roux limb stasis, which predisposes to intussusception [6, 7].
Increased weight loss has also been implicated as a risk factor for developing jejunojejunal intussusception after RYGB. Patients with jejunojejunal intussusception lost 75% of excess weight, versus the overall average of 58% excess weight loss after RYGB [2]. Corresponding thinning of the mesentery is proposed to result in less resistance to invagination and possibly contributes to the development of this pathology [8]. This also explains the delayed presentation after RYGB [4]. These findings are consistent with our patient, who lost 65% of excess body weight over the course of 7 years prior to development of intussusception, currently BMI 31.
The spectrum of surgical management for intussusception at the enteroenteric anastomosis after RYGB ranges from simple reduction to revision of the anastomosis. Any indication of irreversible ischemia on radiographic imaging or intraoperative exploration necessitates resection with subsequent revision of the anastomosis. In the absence of ischemia, multiple modalities remain available. Simper et al. found 100% recurrence rate with reduction alone, 40% recurrence with plication, and 12.5% recurrence rate with resection and revision of the enteroenteric anastomosis [3]. This would suggest that revision of the anastomosis is preferred; however, revision of the anastomosis has corresponding complications of small bowel resection. Therefore, we prefer to simply pexy the small bowel and avoid resection of small bowel, if possible. Varban et al. did not have any recurrence of intussusception on patients undergoing simple reduction without resection during their median 9-month follow-up period [2].
Current literatures notes multiple day hospital courses for these patients [2]. Our experience demonstrates that uncomplicated intussusception at the enteroenteric anastomosis after RYGB can be successfully managed with enteropexy. Although retrograde jejunojejunal intussusception is the most common variant observed in this population, we recommend enteropexy of both antegrade and retrograde portions of this anastomotic junction.
In conclusion, laparoscopic enteropexy is a successful, accessible, and minimally invasive management modality for uncomplicated jejunojejunal intussusception after Roux-en-Y gastric bypass allowing same-day discharge with return to work and activities of daily living without recurrence of intussusception.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Informed consent was provided by patient for publication of this case report and all accompanying medical history and images. Institutional review board approval not indicated.
DISCLOSURES
Dr Kalmar has no relevant financial or nonfinancial relationships to disclose.
Dr Lucktong has no relevant financial or nonfinancial relationships to disclose.



