-
PDF
- Split View
-
Views
-
Cite
Cite
Shahinda Al-Anwar, Alan Askari, Atif Alvi, Right Iliac fossa pain due to torsion and ischaemia of accessory liver lobe, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz101, https://doi.org/10.1093/jscr/rjz101
Close - Share Icon Share
Abstract
An accessory liver lobe (ALL) is the presence of ectopic hepatic tissue which has developed as a result of excessive hepatic development. The majority of patients with ALL remain asymptomatic and their findings are incidental, either after undergoing radiological imaging or during surgery for other pathology. However, in a small number of patients who have a pedunculated ALL, torsion of the lobe on its axis can cause pain, often due to ischaemia of the lobe. We report a 26-year-old female who presented with right iliac fossa pain mimicking acute appendicitis and preceded by recent vigorous exercising activity.
INTRODUCTION
An accessory liver lobe (ALL) is the presence of ectopic hepatic tissue which has developed as a result of excessive hepatic development. Patients in whom these ectopic tissues are found are often entirely symptomatic and the accessory lobe is only discovered when patients have imaging or surgery for other reasons. In a small group of patients, however, ALL can cause pain and abdominal symptoms usually as the lobe torts or otherwise becomes ischaemic.
CASE REPORT
A previously medically fit and well 26-year-old female attended hospital through the Emergency Department after experiencing a 24-hour history of Right Iliac Fossa (RIF) pain associated with nausea and vomiting. There was no previous history of gynaecological, urological disease or previous abdominal surgery. On examination, the abdomen was soft, however, a tender mass was palpable in the RIF. The initial diagnosis was acute appendicitis/appendix mass. Blood analysis demonstrated a white cell count (WCC) of 10.4 × 109/l and a C-Reactive Protein of 11 mg/l, the renal and liver function tests were both normal, the urine was clear and pregnancy test negative.
An ultrasound scan (USS) was performed and a 9 cm mass was demonstrated. A subsequent computer tomography (CT) scan confirmed the mass (Fig. 1) and raised the possibility that the mass may be a small bowel neuroendocrine tumour. The mass reported as separate from the appendix and caecum and no evidence of appendicitis. On the following day, the images were presented, the case was discussed at the colorectal multi-disciplinary team (MDT) meeting and a collective decision was made to perform a magnetic resonance imaging (MRI) scan which the patient underwent the following day. MRI was performed to specifically define the anatomy of the small bowel and its relation to the mass, as this was not clear on CT imaging. Ultimately, the MRI demonstrated a mass with vascular pedicle arising from the inferior aspect of the right hepatic lobe and the appearance raise the possibility of an exophytic liver lesion which has undergone torsion (Fig. 2). She was taken for a diagnostic laparoscopy the next day however given the size of the mass and the slim body habitus of the patient, a decision was made to convert to lower midline mini laparotomy.
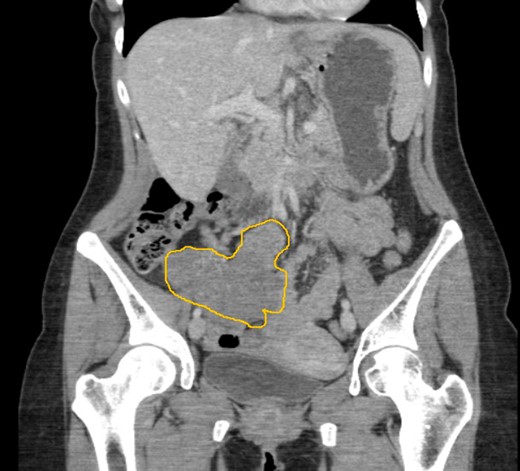
CT imaging demonstrating a 9 cm lesion in the right iliac fossa, displacing adjacent small bowel.

MRI images demonstrating ALL with vascular pedicle attached to liver.
At laparotomy, the mass had the appearance of hepatic tissue with a pedicle attaching it to the liver (Fig. 3). However, it was rotated on its axis (360 degrees), appeared globally ischaemic with patches of necrosis despite its untwisting. The pedicle of the mass was clamped, transfixed and excised. The mass was sent for histopathology which identified it to be an ALL.
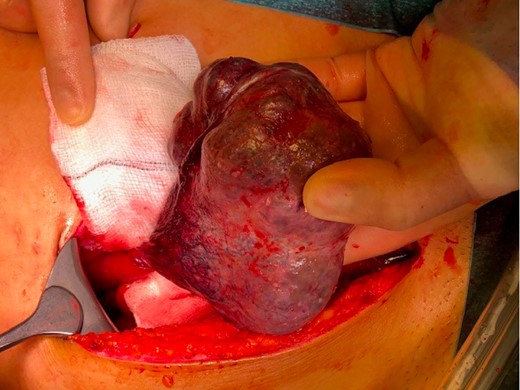
ALL with torted vascular pedicle causing ischaemia of the lobe.
DISCUSSION
ALLs develop as a result of the malformation of the endodermal caudal foregut and segmentation of the hepatic bud in the third gestational week. ALLs may prevent the fusion of the anterior abdominal wall and are therefore frequently associated with anterior abdominal wall defects [1–3]. The accessory lobes are variable in location but are usually located at the right lobe of the liver and attached by a bridge of hepatic tissue, mesentery or a stalk. However, they inherently differ from other ectopic liver tissues by the lack of the continuity with the liver [4].
Classification
ALLs are classified based on the size and their attachments to the liver: big accessory hepatic lobe (>30 g), small accessory hepatic lobe (<30 g), ectopic lobe with no liver connection and microscopic accessory lobe in the gall bladder wall [5]. Another type of classification is based on the biliary drainage and the presence or absence of a common capsule: either a separate accessory lobe duct drains into the intrahepatic or extrahepatic bile duct of the normal liver; or the accessory lobe and the normal liver have a common capsule and the bile duct of the accessory lobe drains into an extrahepatic duct [5].
Clinical features
Patients with uncomplicated ALL are usually asymptomatic but may occasionally present with acute or recurrent abdominal pain, precordial pain, nausea, vomiting or fluctuating impaired liver function [6, 7]. The clinical manifestation of an ALL depend on the complications, such as torsion, trauma, rupture, or infarction. Torsion occurs most frequently with the patient presenting with right sided abdominal pain with or without palpable mass. Often, torsion of ALL is misdiagnosed as any of the acute abdomen differentials or intra-abdominal tumours. It may be caused by strenuous exercise, as in our patient, or trauma [8]. Associated umbilical hernia or bile cysts increases the suspicion of torsion ALL [9]. ALL may also revert, infarct, rupture, fracture or bleed. They may also cause haemangiomas, biliary atresia, gall bladder torsion and hepatic dysfunction [7].
Diagnosis
ALL may appear as an undetermined mass on imaging, however, visualization of the anatomic connection of the ALL to the liver can be appreciated through the use of CT or MRI. In our case the MRI was more sensitive than the CT scan in establishing the diagnosis. The presence of independent biliary drainage as well as arterial, venous and portal branches should arouse suspicion of this rare anomaly. In case of torsion the appearance might be more difficult because of the lack of visualization of the vascular pedicle. Enhanced CT scan usually shows vascularization defects, loss of normal architecture of liver parenchyma, and uncertain origin of the mass which may be confused with extrahepatic tumours of pancreatic, ovarian, or peritoneal origin or an acute inflammatory condition (e.g. cholecystitis and appendicitis). On ultrasonography, a twisted ALL appears as an hypoechogenic mass caused by congestion, and on colour Doppler ultrasonography, it appears to be without vascular supply.
ALL is a rare congenital anomaly and is difficult to diagnose both clinically and radiologically. Prompt history and physical examination is important as is definitive radiological imaging such as CT or MRI.
CONFLICT OF INTEREST STATEMENT
None declared.



