-
PDF
- Split View
-
Views
-
Cite
Cite
Moaath Al Smady, Nurul Nadia Binti Zahari, Noor Syahirah Binti Mohd Sahid, Nurul Syuhada Binti Saparudin, Anterior mediastinal teratoma with pericardial effusion. Rare presentation, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz136, https://doi.org/10.1093/jscr/rjz136
Close - Share Icon Share
Abstract
Mediastinal teratoma is an uncommon finding in the pediatric age group, accounting for only 7–11% of extragonadal teratomas. Rarely, the tumor can rupture and erode into the pericardium or pleural space. However, pericardial effusion due to rupture is infrequent. We report a case of such a rare presentation in a 10-year-old young female. The patient underwent a mediastinal tumor excision. Histopathology revealed that there was ruptured mature cystic teratoma with inflammatory reaction. Numerous cases of mediastinal teratoma with pericardial effusion have been reported but only few have been presented in the pediatric age group.
INTRODUCTION
Mediastinal teratomas are an extragonadal germ cell tumor, originating from pluripotent cell with the multi-directional potential of differentiation into different types of cell [1]. We aim to report the clinical and pathological findings of this case in order to evaluate the treatment and the long-term biological behavior. Herein, we report a case of successful surgical management of an anterior mediastinal teratoma in a child.
CASE REPORT
A 10-year-old female patient was well prior to an evaluation for chest pain of two weeks duration, at which an anterior mediastinal mass, was noted on chest radiograph. Chest X-ray (Fig. 1) showed a well-defined homogenous opacity in the right upper and mid zones extending from mediastinum and obliterating the hilar shadow. Transthoracic echocardiography revealed a pericardial effusion. Chest CT (Fig. 2) revealed a well-defined tumor mass involving the anterior mediastinum adjacent to the heart measuring 6 × 4 cm. Mild amount of pericardial fluid noted.


The CRP level was significantly elevated with 51.27 mg/l. Echinococcal test found negative. The serum alpha fetoproteinwas 5 ng/ml(reference range.89–8.78 ng/ml), and β-human chorionic gonadotropin serum levels were 3 IU/l normal range less than10 IU/l.
Pre-operative working diagnosis was symptomatic anterior mediastinal tumor either pericardial cyst or teratoma with pericardial effusion.
She underwent mediastinal tumor excision, thymectomy and partial pericardectomy through midsternotomy. Pericardium was not reconstructed because small defect around 2 cm.
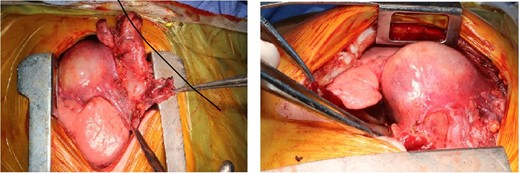
The mass was attached to pericardium, compressing the right atrium and encased the right phrenic nerve (Fig. 3). The mass en-bloc excision and thymectomy revealed multiloculate well-defined cyst measuring 6 cm in maximum dimension. Upon opening the cyst, and the pericardium yellowish sebaceous and cheesy material was found and identified as ruptured mature cystic teratoma with inflammatory reaction. Microscopy showed a ruptured mature cystic teratoma with inflammatory reaction (showing an unremarkable squamous, respiratory and gastric types epithelium, mature adipose tissue, smooth muscle tissue, and skin adnexa), with an unremarkable thymic tissue and no immature elements or malignancy.
Pericardium biopsy sections show vascularized fibrous tissue with congestion and mild inflammation lined by unremarkable mesothelial cells. Patient underwent uneventful recovery and upon follow-up no clinical or radiological signs of recurrence.
DISCUSSION
Teratoma is a rare type of germ cell tumor that arises from immature primordial germ cells and can be localized either in the gonads or in an extra-gonadal position, at or near the midline. It originates from two to three germ cell layers. The accepted theory is that they arise from an error in migration of a multipotent germ cell along the urogenital ridge to the gonad during early embryogenesis [2]. The most common reported site for extragonadal teratoma is the anterior mediastinum [3]. Histologically, it is classified as mature; immature; teratoma with malignant transformation; seminoma; and nonseminoma. The patient in our case had mature cystic teratoma located in the anterior mediastinum. Mediastinal mature teratoma is a benign, slow growing neoplasm. The incidence of teratoma worldwide is 1 in 4000 live births [4]. The common age of presentation is young adults with mean age of 20–40 years old. This case uniquely illustrates a very young patient of 10-year-old. Most patients with mediastinal mature teratoma are asymptomatic and in this case the tumor was found incidentally on a chest x-ray. When symptoms are present, it is due to the compression of surrounding structures. These include chest pain, dyspnea, cough and respiratory distress. Occasionally the tumor can rupture and erode into the tracheobronchial tree, pericardium or pleural space, subsequently causing hemoptysis and trichoptysis which is pathognomonic for teratoma [5]. This results in significant complications. In the case being discussed, the patient had a history of left-sided chest pain and heaviness, without cough or dyspnea. The patient had unusual presentation in the form of pericardial effusion and this is an extremely rare consequence of ruptured teratoma. Chest CT is the imaging technique of choice in the evaluation of the abnormal mediastinum. It shows the location and extension of the mass in relation to the adjacent structure as well as to detect hypervascularization of the mass. The typical appearance is heterogenous, sharply marginated, lobulated neoplasms and intrinsic elements of the lesion, including soft tissue, fat, areas of cystic calcifications, and fat fluid which is pathognomonic for diagnosing teratoma [6]. It can also show findings of ruptured teratoma, which consist of heterogeneity of the mass, fat globules at the rupture site, consolidation or atelectasis in the adjacent lung, and effusion. In comparison to our case, the CT scan shows multiloculated pericardial cysts containing yellowish sebaceous materials. A chest X-Ray typically reveals a rounded, well-circumscribed, lobulated calcification protruding against the adjacent lung. This combination of findings is consistent with our case. Visualizations of well-formed tissues such as teeth and hair are pathognomonic. MRI is useful to further evaluate the mass infiltration. It will reveal the heterogenous signal intensity containing mixtures of fat, water, soft tissue, and calcifications. Fortunately for this patient, no invasions of adjacent structures were found. Hence, no complication ensues. CT-guided biopsies are usually done to determine whether the tumor was malignant or benign. The diagnostic biopsy, either by thoracoscopic or open surgery, may be indicated to determine the specific germ cell tumor. Therefore, open surgery through median setrnotomy was done on the patient and we found it was a ruptured cystic teratoma with inflammatory reaction without any elements of immaturity or malignancy. Involvement of pericardium is considered a life-threatening condition which emphasizes the need for urgent intervention. Complete surgical excision is the treatment of choice for mediastinal teratoma. It helps in establishing the diagnosis as well as ensuring a long-term cure rate with little chance of recurrence. The most commonly performed method is median sternotomy due to excellent exposure. If it affects the hemithorax, lateral thoracotomy is selected instead [7]. In malignant teratoma, combination with chemotherapy can improve survival [1]. Median sternotomy is the surgical approach of choice for this case. Since mature teratomas are benign tumors, it has excellent prognosis.
CONCLUSION
In dealing with the anterior mediastinal mass, we must consider the possibility of involving the adjacent structure while planning the best treatment. The surgical approach must suit the extent and size of the tumor to ensure a safe dissection of the tumor.
CONFLICT OF INTEREST STATEMENT
None declared.



