-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Gray, David Lewis, Surviving complete gastric infarction in remote Australia, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz133, https://doi.org/10.1093/jscr/rjz133
Close - Share Icon Share
Abstract
Gastric volvulus is a potentially lethal condition with mortality rates reported up to 50%. The high mortality rate is largely due to the rarer complication of gastric infarction, the diagnosis of which is often difficult. From the small series published, it is known that delays to receiving definitive surgical intervention negatively impacts patient outcomes. We present a case of long-term survival of a 69-year-old man who presented to his local hospital in remote Australia with gastric volvulus and complete gastric infarction. His initial management was delayed as he could not undergo life-saving surgery at his presenting hospital. He was transferred to the regional referral hospital and survived both an upfront damage-control oesophagogastrectomy and then transfer to a metropolitan centre for alimentary tract reconstruction. He was alive and living at home without major postoperative morbidity 12 months later.
INTRODUCTION
Gastric volvulus is a potentially lethal condition with mortality rates reported up to 50%. The high mortality rate is largely due to the rarer complication of gastric infarction and swift surgical intervention is crucial once suspicion of gastric strangulation has been raised. We present the first reported case of long-term survival following multiple inter-hospital transfers of a patient with complete gastric infarction.
CASE REPORT
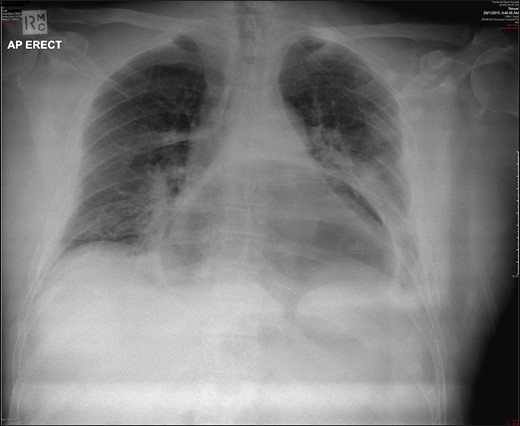
A 69-year-old man with a background medical history significant for hypertension and mild obesity, presented to his local district hospital in remote New South Wales, Australia with sudden onset of severe epigastric pain radiating to his back. He was diaphoretic and pale, and initial assessment of the patient seemed to be that of a man suffering an acute myocardial infarction. Despite this, his initial observations were all within normal limits, and his electrocardiograph revealed a sinus bradycardia and no ischaemic changes. All initial blood examinations, including serum troponin, lactate, liver function tests, renal markers, electrolytes and C-reactive protein were completely normal, with the full blood count revealing only a mild leucocytosis (12.3 × 109/L). Interestingly, the most significant finding came from his initial chest X-ray which showed a large intrathoracic gastric bubble consistent with a large hiatus hernia (Fig. 1). The patient went on to have an intravenous contrast-enhanced computed tomography (CT) scan of the chest and abdomen which revealed an obstructed intra-thoracic stomach incarcerated within a para-oesophageal hernia (Fig. 2). Surgical services in the patient’s local town are limited and thus the patient was transported to the closest regional centre with on-call general surgical services. Decompression with a nasogastric tube (NGT) was attempted but failed.
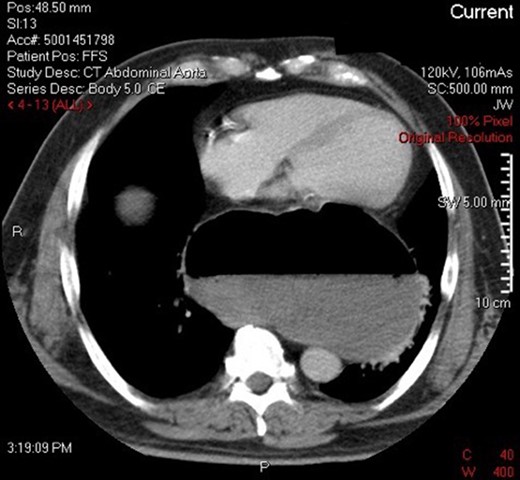
CT demonstrating obstructed intra-thoracic stomach in mesenteroaxial alignment.
The patient arrived late in the evening to the regional centre and despite suffering from ongoing pain, had normal haemodynamic observations – he was subsequently admitted to the ward. Deterioration in his clinical condition occurred swiftly the following morning, and surgical intervention was urgently arranged. A damage-control laparotomy was performed and confirmed the diagnosis of an incarcerated para-oesophageal hernia with complete infarction of the stomach and lower oesophagus (Fig. 3) secondary to a mesenteroaxial gastric volvulus. An emergency oesophagogastrectomy with excision of the gastro-oesophageal junction and distal four centimetres of oesophagus was performed. The patient survived the procedure, his critical condition steadied, and he was able to be transferred to an Upper Gastrointestinal surgery unit at a tertiary metropolitan centre for Roux-en-Y oesophago-jejunostomy reconstruction. The reconstruction occurred three days after the patient’s initial laparotomy and was complicated by a small anastomotic leak which was managed conservatively. The leak healed slowly and the patient was eventually discharged home in a reasonable state of health a total of eight weeks after the initial presentation. He remains well and at home twelve months after his initial presentation with gastric volvulus.
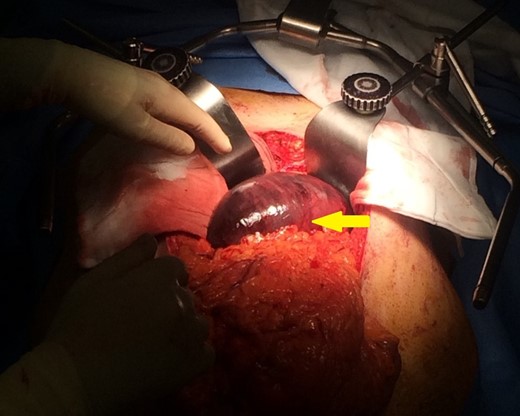
Intraoperative photograph identifying infarction of the greater curvature of the stomach.
DISCUSSION
Gastric volvulus is a rare condition compromising abnormal rotation of the stomach along its longitudinal (organoaxial) or transverse (mesenteroaxial) axis. Organoaxial volvulus is the most common occurring in 60% of cases and is characterized on CT by the greater curvature of the stomach coming to rest superior to the lesser curvature, resulting in an ‘inverted’ stomach [1]. The second type of gastric volvulus is mesenteroaxial as found in the case study. This less commonly encountered variant (occurring approximately 29% of the time) [2] is characterized by rotation of the stomach along an axis perpendicular to its longitudinal axis. In this position the stomach lies in the vertical plane with the antrum and pylorus rotated anterior and superior to the gastroesophageal junction [3]. A third type exists which is a combination of the previous two [3]. Gastric volvulus may be primary or secondary. The primary (or idiopathic) subtype occurs due to a laxity of the supporting ligaments of the stomach, thereby allowing the stomach to twist along its mesentery [4]. Secondary gastric volvulus is most commonly seen, as in this case, in relation to a para-oesophageal hernia, but may also be seen in the context of gastric neoplasia or upper abdominal adhesions [5]. Acute gastric volvulus classically presents with a triad of severe epigastric pain, vomiting, and difficulty or inability to pass a nasogastric tube [4]. It is a surgical emergency, due to the risk of gastric ischaemia, with mortality rates of between 30-50% regularly quoted in the literature [6].
The case presented is of particular interest as although mortality with gastric strangulation is high, the stomach has a rich blood supply and therefore ischaemic events of this nature occur in less than 10% of patients. The diagnosis of which patients fall into this group, and thus require urgent life-saving surgery, is ultimately the most difficult question in their management [7]. Of particular note in this case, factors identified by Light et al. as being critical to patient survival, namely early NGT decompression and early transfer to the operating room, did not occur – nevertheless the patient survived [8]. This is the only reported case of long-term survival following multiple inter-hospital transfers of a patient presenting with complete gastric infarction.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST STATEMENT
None declared
CONFLICTS OF INTEREST OR FUNDING TO DISCLOSE
None.



