-
PDF
- Split View
-
Views
-
Cite
Cite
Basel Ahmad, Ahmed Alshammat, Alin Haya Hamed, M Fadi Alkurdi, Hamoud Hamed, Pancreaticoduodenectomy in a patient with a rare celiac trunk and hepatic artery anomaly, a case report from Syria, Journal of Surgical Case Reports, Volume 2019, Issue 5, May 2019, rjz148, https://doi.org/10.1093/jscr/rjz148
Close - Share Icon Share
Abstract
Pancreaticoduodenectomy is still one of the biggest and high complicated surgeries. It still has high morbidity and mortality rates. liver receives its blood supply from one hepatic artery a branch of the celiac trunk However variations of hepatic and celiac trunk are not rare. We present a case of a 60-year-old patient who underwent pancreaticoduodenectomy for ampulla tumor in which there were some rear anomalies. Angiographic CT after procedure confirmed the absence of celiac trunk, the absence of left gastric, the splenic artery arising from aorta directly and common hepatic artery arising from superior mesenteric artery. These anomalies are not considered contraindication and should not be. with good surgical experience the procedure may be done safely giving the patient his last choice to fight the disease.
INTRODUCTION
Pancreaticoduodenectomy (PD) is one of the biggest and high complicated surgery. It still has high morbidity and mortality rates [1].
Normally, liver receives its blood supply from one hepatic artery a branch of the celiac trunk and a pancreaticoduodenal arcade between superior mesenteric artery (SMA) and hepatic artery (HA) [2].
However, this normal supply apply only for 50-60% of cases [2] and variations of hepatic and celiac trunk are not rare [1].
These variations may complicate the procedure more and could lead to serious complications as biliary fistula, hepatic ischemia, hemorrhage and liver abcesses [1, 3].
Many surgeons have studied these anomalies in detailed and Michel’s classification is probably the most used one [1].
We present a case of a 60-year-old patient who underwent pancreaticoduodenectomy for ampulla tumor and had a very rare anomaly in the celiac trunk and hepatic artery.
CASE REPORT
A 60-year-old patient with no medical history but diabetes mellitus II was referred to our tertiary university hospital (Al-Assad university hospital for intermittent jaundice.
The complaint started one year before, in which the patient suffered fatigue and general weakness without weight loss or changes in bowel movement.
One month before admission, he developed pain in the right upper quadrant and intermittent jaundice as well as fatigue and general weakness.
On admission, the patient had no symptoms, no jaundice the lab values are shown on (Table 1).
| Test . | Result . | Reference range . |
|---|---|---|
| White blood cells | 6.29 | 4400–11 000/μl |
| Neutrophils percent | 62% | 40–70% |
| Hemoglobin | 12 | 13–16 g/dl |
| Hematocrit | 37.5 | 38–53% |
| Platelets | 267 | 150–450 × 103/ μl |
| Urea | 24 | 10–50 mg/dl |
| Creatinin | 0.9 | 0.7–1.36 mg/dl |
| ALT | 26 | 8–20 IU/l |
| AST | 18 | 8–20 IU/l |
| PT | 88% | |
| CEA | 1.45 | Up to 3,non smokers up to 6, smokers |
| CA19_9 | 2.28 | 0–37 |
| AFP | 1.33 | 0–10.9 |
| Test . | Result . | Reference range . |
|---|---|---|
| White blood cells | 6.29 | 4400–11 000/μl |
| Neutrophils percent | 62% | 40–70% |
| Hemoglobin | 12 | 13–16 g/dl |
| Hematocrit | 37.5 | 38–53% |
| Platelets | 267 | 150–450 × 103/ μl |
| Urea | 24 | 10–50 mg/dl |
| Creatinin | 0.9 | 0.7–1.36 mg/dl |
| ALT | 26 | 8–20 IU/l |
| AST | 18 | 8–20 IU/l |
| PT | 88% | |
| CEA | 1.45 | Up to 3,non smokers up to 6, smokers |
| CA19_9 | 2.28 | 0–37 |
| AFP | 1.33 | 0–10.9 |
| Test . | Result . | Reference range . |
|---|---|---|
| White blood cells | 6.29 | 4400–11 000/μl |
| Neutrophils percent | 62% | 40–70% |
| Hemoglobin | 12 | 13–16 g/dl |
| Hematocrit | 37.5 | 38–53% |
| Platelets | 267 | 150–450 × 103/ μl |
| Urea | 24 | 10–50 mg/dl |
| Creatinin | 0.9 | 0.7–1.36 mg/dl |
| ALT | 26 | 8–20 IU/l |
| AST | 18 | 8–20 IU/l |
| PT | 88% | |
| CEA | 1.45 | Up to 3,non smokers up to 6, smokers |
| CA19_9 | 2.28 | 0–37 |
| AFP | 1.33 | 0–10.9 |
| Test . | Result . | Reference range . |
|---|---|---|
| White blood cells | 6.29 | 4400–11 000/μl |
| Neutrophils percent | 62% | 40–70% |
| Hemoglobin | 12 | 13–16 g/dl |
| Hematocrit | 37.5 | 38–53% |
| Platelets | 267 | 150–450 × 103/ μl |
| Urea | 24 | 10–50 mg/dl |
| Creatinin | 0.9 | 0.7–1.36 mg/dl |
| ALT | 26 | 8–20 IU/l |
| AST | 18 | 8–20 IU/l |
| PT | 88% | |
| CEA | 1.45 | Up to 3,non smokers up to 6, smokers |
| CA19_9 | 2.28 | 0–37 |
| AFP | 1.33 | 0–10.9 |
Ultrasound showed common biliary duct dilation 2 cm, intrahepatic biliary system dilation. ERCP then was indicated in which swollen ampulla was detected, dilated common biliary duct 2 cm, dilation of intra hepatic ducts, signs of which increased the suspicion of ampulla tumor, so the ampulla was cut, biopsies were taken and 8.5 plastic stent was administrated.
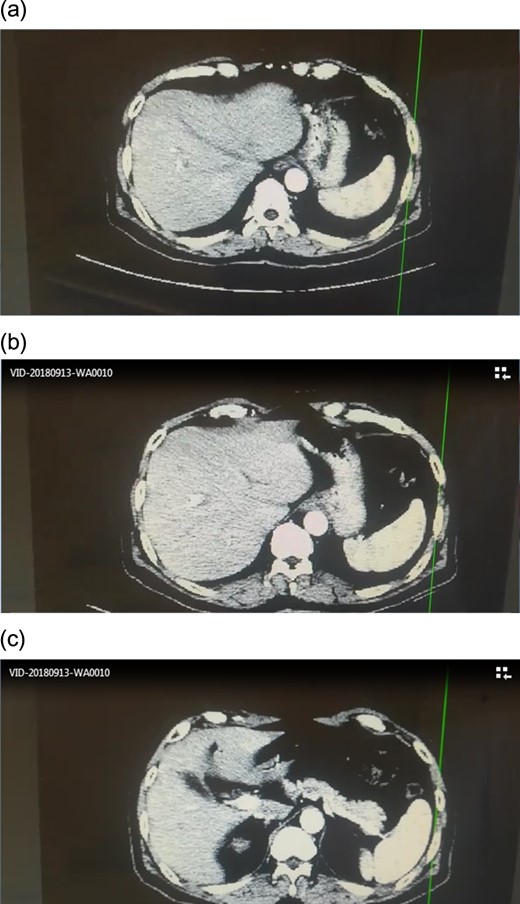
CT scan showed no signs of metastasis (Fig. 1).
ERCP biopsy came out: villous adenomatous of ampulla vater with focal mild to moderate dysplasia. Thus the patient was being prepared for whipple procedure.
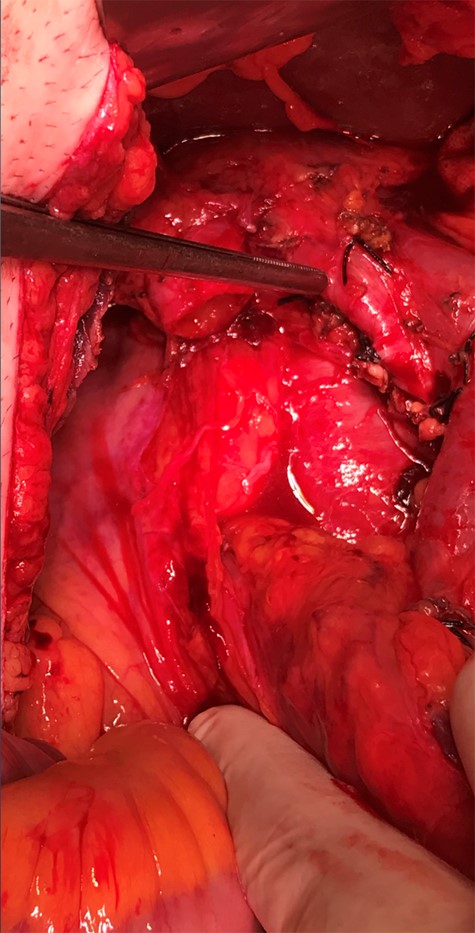
In operating room, Kocher incision, no ansarca, no peritoneal metastasis, the decision to perform whipple procedure was made. Gallbladder was resected, kocher maneuver, when isolating the CBD and common hepatic artery, anomalies were found, and the artery system was not that clear, no clear celiac trunk and no clear common hepatic artery. (Fig. 2)
Decision to continue whipple procedure was made, and slow and careful ligation of arteries was performed. Hopefully, the surgical team managed to make the procedure done.
Final pathology report: adenocarcinoma of the ampulla grade 1, duodenal gastric and pancreatic surgical margins were free, all isolated lymph nodes were free 0/18, the lymph nodes are free pT1a, Pn9, Mx.
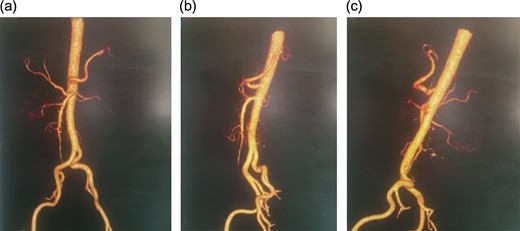
Angiographic CT after procedure confirmed the absence of celiac trunk, the absence of left gastric, the splenic artery arising from aorta directly and common hepatic artery arising from superior mesenteric artery.(Fig. 3)
The patient was discharged one week later with 2 days in ICU,. 6 month follow-up revealed a healthy patient with no recurrence or ischemic complication.
DISCUSSION
It is a fact that it is hard even for experienced surgeons to perform major surgeries, such as liver resection, liver transplant or pancreaticoduodenectomy,these surgeries challenge the surgeons at their best [1].
only 52–80% of all cases has normal hepatic arterial anatomy in which the celiac trunk gives the splenic, the common hepatic and the left gastric branches [1].
As these anomalies are not rare, many has already studied and documented them and Michel’s classification may be the most acceptable and used one in the surgery world these days [1].
‘replaced’ and ‘accessory‘ hepatic artery anomaly were stressed up in Michel’s classification due to its impact on liver transplant and pancreaticoduodenectomy surgeries [1].
Bifurcation of Celiac trunk, gastrosplenic trunk and hepatosplenic trunk are the most common anomalies whereas an absent celiac trunk is too rare and Bergman et al. have only reported it in his study as 0.4% [1].
In our case, there was no celiac trunk, no left gastric artery, the splenic artery emerged directly from the aorta and the common hepatic artery arising from Superior mesenteric artery. The surgical team completed the procedure despite this anomaly. The patient had a good recovery and a six-month follow up showed a person in acceptable health with no recurrence.
Zhou Ye et al. reported in 2017 a case of a patient who underwent pancreaticoduodenectomy and The CHA emerged from the superior mesenteric artery, the left gastric artery and splenic artery arising from the anterior wall of the abdominal l aorta [1].
CONCLUSION
Pancreaticoduodenectomy (PD) is one of the biggest and high complicated surgery. It still has high morbidity and mortality rates
variations of hepatic and celiac trunk are not rare and These variations may complicate the procedure more and could lead to serious complications. However, they are not considered contraindication and with good surgical experience the procedure may be done safely giving the patient his last choice to fight the disease.
CONFLICT OF INTEREST STATEMENT
None declared.



