-
PDF
- Split View
-
Views
-
Cite
Cite
John Alfred Carr, The Dudley colectomy in urgent and emergent situations: a 10 patient case series, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz123, https://doi.org/10.1093/jscr/rjz123
Close - Share Icon Share
Abstract
Left-sided colon pathology that needs to be treated in an emergency situation usually requires a partial colectomy and colostomy with a Hartmann’s pouch. Primary anastomosis is avoided with an unprepped left colon due to the risk of post-operative anastomotic leakage. In this series, 10 patients were treated with on-table lavage to wash out the colon, and left colectomy with primary anastomosis in urgent and emergent situations without a protective ileostomy (the Dudley colectomy). All patients acutely recovered and none had an anastomotic leak. There was a single superficial wound infection, and a single late mortality due to heart failure. On-table colonic lavage and left colectomy with primary anastomosis without a protective ileostomy is a safe and effective way to treat left-sided colon emergencies without a protective ileostomy.
INTRODUCTION
The standard of care to treat perforated diverticulitis with peritonitis, or any left-sided colon emergency, is still a colectomy with an end colostomy and a rectal Hartmann’s procedure. Another accepted, but less often used, procedure is a left colectomy with a primary colorectal anastomosis and a protective diverting ileostomy. These two procedures were just compared at the end of 2017 in a prospective, randomized multicenter trial, the DIVERTI trial, which was recently published [1]. The idea of performing a primary anastomosis using unprepped colon without an ostomy has never been widely accepted, although some authors are advocating that it may be a safe option [2–4]. Fear of an anastomotic leak from an unprepped colon has so far prevented its widespread acceptance.
Certainly, both patients and surgeons wish to avoid a colostomy; and, one-stage treatment of acute left-sided colon pathology is possible and can be safely performed using the technique of on-table colonic lavage and anastomosis as originally described by Dudley in 1980 [5]. This technique preps the colon quickly and allows a safe anastomosis in a one-stage operation. However, it is generally not used in emergent situations due to an increased length of time required to lavage the colon. The purpose of this article is to describe the improved contemporary technical details and outcome in a small case series of patients who were able to avoid a colostomy and have definitive treatment of acute left-sided colon pathology with this single operation in emergent situations.
CASE REPORT AND TECHNIQUE
After induction of anesthesia, the patient is placed into the high lithotomy position and digital rectal exam is performed to remove any fecal matter and then the rectum is washed with 200–250 cc of saline to flush out the fecal debris. Digital rectal exam is repeated to remove any stool that has been flushed downwards. This process is repeated four to five times until the saline return is clear and the rectum is empty (Fig. 1).
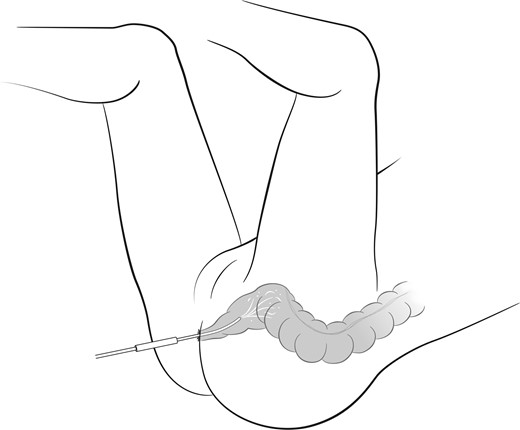
Rectal lavage to wash out the rectum and prevent fecal contamination of the pelvic anastomosis.
The patient is then prepped and draped and the legs are lowered to a low lithotomy position. A full laparotomy incision is made and a standard left colectomy is performed, being sure to remove all diverticular disease or pathology.
After resection of the left colon, sterile corrugated ventilator tubing (King Systems, Noblesville, IN, USA) is inserted into the open end of the colon at least 4 cm. Umbilical tape is used to secure the tubing within the colon. The other end of the tubing is thrown off the field into a kick bucket or large basin on the floor.
The tip of the appendix is cut off and a 12-16 French Foley catheter is inserted through the appendix into the cecum and the balloon is inflated and pulled back. If the patient does not have an appendix, two 2-0 silk sutures are sewn in purse string fashion, one inside the other, as circles around an anterior position on the cecum. The cecum is then punctured within the two circular sutures and the Foley is inserted into the cecum and the sutures snugged down with Rummel tourniquets.
A three liter bag of warm saline is then connected to the Foley and instilled into the colon. The terminal ileum is manually occluded. As the colon fills with saline, liquid feculent material and often solid chunks of stool will begin to flush out the other end. The entire three liter bag is flushed though until the fluid in the ventilator tubing is seen to be coming out clear (Fig. 2).
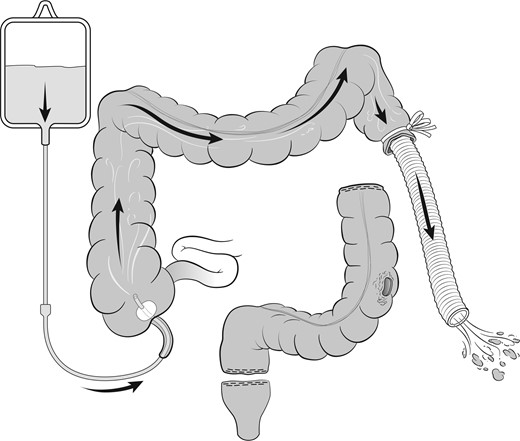
Colonic lavage cleansing the colon and extent of resection shown prior to anastomosis.
The Foley is then removed and an appendectomy is performed. The umbilical tape is cut off the colon and the ventilator tubing discarded. The anvil of a 33 EEA stapler (Ethicon Endo-Surgery, Cincinnati, OH) is passed into the cut end of colon and a 2-0 Prolene purse string suture is sewn to secure the anvil. It is important that the anastomosis be performed to the true rectum, and not the lower sigmoid colon. Only the true rectum can be reliably washed-out with the preoperative rectal lavage and prevent stool from being pushed into the anastomosis with the EEA stapler.
The mobilized transverse colon is brought down to the rectum without tension and a standard EEA anastomosis is created. Flexible colonoscopy is used to inspect the anastomosis from within. The pelvis is filled with saline and the colon is insufflated via the colonoscope to check for air leakage. The abdomen is then closed. With this technique, ‘protective’ diverting ileostomies are not used.
Patients
The indications to perform this procedure, rather than give the patient a colostomy, were patient refusal to have a colostomy, the patient was mentally incapable of caring for a colostomy, or the patient’s lifestyle was such that colostomy care would be impossible.
Ten patients were treated emergently using this method, ranging in age from 25 to 86. Patient details are given in Table 1. The most common indication for surgery was perforated diverticulitis with peritonitis. Three patients (30%) were hemodynamically unstable at the time of surgery. After the anastomosis was completed and colonoscopy was performed, all ten patients were found to have a clean and empty rectum and colon proving the lavage was very effective. The lavage portion of the operation required an average 27 minutes (range 22–36, SD ± 6 minutes). There was a single superficial incisional infection, and a single late mortality occurred due to heart failure. The mean length of stay was 6 days (range 4–8, SD ± 2 days). There were no instances of anastomotic complications, no anastomotic leaks, and no deep infectious complications occurred.
| n . | Age . | Pathology . | Hemodynamics . | Complications . | Anastomotic leak . |
|---|---|---|---|---|---|
| 1 | 86 | Perforated diverticulitis | Stable | None | No |
| 2 | 67 | Perforated diverticulitis | Stable | None | No |
| 3 | 49 | Perforated diverticulitis | Stable | None | No |
| 4 | 31 | Perforated diverticulitis | Stable | None | No |
| 5 | 75 | Diverticular hemorrhage | Unstable | None | No |
| 6 | 25 | Gun shot through colon | Stable | None | No |
| 7 | 65 | Late polypectomy bleed | Unstable | Wound infection | No |
| 8 | 41 | Perforated diverticulitis | Stable | None | No |
| 9 | 57 | Diverticular hemorrhage | Unstable | Heart failure/death | No |
| 10 | 68 | Perforated diverticulitis | Stable | None | No |
| n . | Age . | Pathology . | Hemodynamics . | Complications . | Anastomotic leak . |
|---|---|---|---|---|---|
| 1 | 86 | Perforated diverticulitis | Stable | None | No |
| 2 | 67 | Perforated diverticulitis | Stable | None | No |
| 3 | 49 | Perforated diverticulitis | Stable | None | No |
| 4 | 31 | Perforated diverticulitis | Stable | None | No |
| 5 | 75 | Diverticular hemorrhage | Unstable | None | No |
| 6 | 25 | Gun shot through colon | Stable | None | No |
| 7 | 65 | Late polypectomy bleed | Unstable | Wound infection | No |
| 8 | 41 | Perforated diverticulitis | Stable | None | No |
| 9 | 57 | Diverticular hemorrhage | Unstable | Heart failure/death | No |
| 10 | 68 | Perforated diverticulitis | Stable | None | No |
| n . | Age . | Pathology . | Hemodynamics . | Complications . | Anastomotic leak . |
|---|---|---|---|---|---|
| 1 | 86 | Perforated diverticulitis | Stable | None | No |
| 2 | 67 | Perforated diverticulitis | Stable | None | No |
| 3 | 49 | Perforated diverticulitis | Stable | None | No |
| 4 | 31 | Perforated diverticulitis | Stable | None | No |
| 5 | 75 | Diverticular hemorrhage | Unstable | None | No |
| 6 | 25 | Gun shot through colon | Stable | None | No |
| 7 | 65 | Late polypectomy bleed | Unstable | Wound infection | No |
| 8 | 41 | Perforated diverticulitis | Stable | None | No |
| 9 | 57 | Diverticular hemorrhage | Unstable | Heart failure/death | No |
| 10 | 68 | Perforated diverticulitis | Stable | None | No |
| n . | Age . | Pathology . | Hemodynamics . | Complications . | Anastomotic leak . |
|---|---|---|---|---|---|
| 1 | 86 | Perforated diverticulitis | Stable | None | No |
| 2 | 67 | Perforated diverticulitis | Stable | None | No |
| 3 | 49 | Perforated diverticulitis | Stable | None | No |
| 4 | 31 | Perforated diverticulitis | Stable | None | No |
| 5 | 75 | Diverticular hemorrhage | Unstable | None | No |
| 6 | 25 | Gun shot through colon | Stable | None | No |
| 7 | 65 | Late polypectomy bleed | Unstable | Wound infection | No |
| 8 | 41 | Perforated diverticulitis | Stable | None | No |
| 9 | 57 | Diverticular hemorrhage | Unstable | Heart failure/death | No |
| 10 | 68 | Perforated diverticulitis | Stable | None | No |
DISCUSSION
Although first described by Dudley in 1980, the technique did not become immediately popular [5]. Possibly because Dr. Dudley was British, the technique gained great favor throughout Britain and was even proposed to become standard treatment for left-sided colon pathlogy in England [6]. Two years later, it was investigated in a prospective, randomized trial throughout England in a multi-center study involving 12 hospitals [7]. The authors concluded that segmental resection with on-table lavage had a better long-term outcome than other procedures, and a low anastomotic complication rate [7]. A designed questionnaire study compared the opinions of the procedure of choice for left-sided colonic emergencies among United States surgeons versus British surgeons [8]. The British surgeons were much more likely to perform resection with on-table colonic lavage and primary anastomosis in patients with sigmoid obstruction or perforation, while the United States surgeons were more likely to perform a colostomy and Hartmann’s procedure (P < 0.0001) [8]
One argument against the procedure is that it adds too much time to the operation, which could be detrimental in a marginally stable patient. This issue was examined in a very large study from Japan in which 715 consecutive patients were treated for left-sided colon cancer. Of these, 101 obstructed patients underwent resection with on-table colonic lavage and primary anastomosis, while 614 unobstructed patients underwent a standard preoperative mechanical bowel preparation. Although these operations were elective and not emergencies, the on-table lavage group’s average operating time was only 28 minutes longer, and anastomotic leak only occurred in 3 (3%) of the lavage patients [9].
Now 39 years after the procedure was introduced, several very large studies totaling 408 patients have proven its safety, with an anastomotic leak rate of 3-6% and a mortality of 2-6%, which compares favorably with the results of a standard left colectomy after preoperative mechanical bowel preparation [9, 10].
CONCLUSION
On-table colonic lavage with left-sided colon resection and primary anastomosis without a diverting ileostomy is a safe and effective way to provide one-stage treatment of left-side colon emergencies and avoid a colostomy.
CONFLICT OF INTEREST STATEMENT
The author has no conflicts of interest and received no financial support to produce this manuscript.



