-
PDF
- Split View
-
Views
-
Cite
Cite
Jude Opoku-Agyeman, Sergio Perez, Amir Behnam, David Matera, Reconstruction of sternoclavicular defect with completely detached pectoralis major flap, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz122, https://doi.org/10.1093/jscr/rjz122
Close - Share Icon Share
Abstract
Sternoclavicular joint infection is very rare. Osteomyelitis is a known complication of septic sternoclavicular joint. Once this condition is diagnosed, aggressive management including antibiotic and surgical debridement is warranted. Patients are often left with sizeable sternoclavicular defects that may need surgical reconstruction. In this report, we describe the use of a completely detached pectoralis major flap for the reconstruction of a large sternoclavicular defect after resection for osteomyelitis. Briefly, after the debridement of the infected sternoclavicular joint, the pectoralis major was detached from its sternoclavicular attachments and further detached from the humeral attachments rendering it completely detached on a vascular pedicle. The muscle was advanced to cover the defect and secured. Patient recovered well without any surgery related complication. She retained good use of the ipsilateral upper extremity. The pectoralis major can be completely detached to provide ample coverage for sternoclavicular joint reconstruction if needed.
INTRODUCTION
Sternoclavicular joint infections are rare. Osteomyelitis is a complication of septic sternoclavicular joint [1]. The diagnosis of this entity mandates aggressive treatment including debridement and antibiotics. Infections of the sternoclavicular joint can lead to subcutaneous abscesses and fistulation to the skin. To date there is very little in the literature describing surgical reconstruction of the sternoclavicular joint. Management of sternoclavicular wound infections have ranged from, local wound care, the use of negative pressure wound therapy, the use of muscle flaps. We describe a case of a patient with a large sternoclavicular defect with associated non-healing cutaneous fistula that underwent an ipsilateral pectoralis pedicle flap closure. To the best of our knowledge, this is the first reported case of the use of a completely detached pectoralis major flap in the reconstruction of a sternoclavicular defect.
CASE REPORT
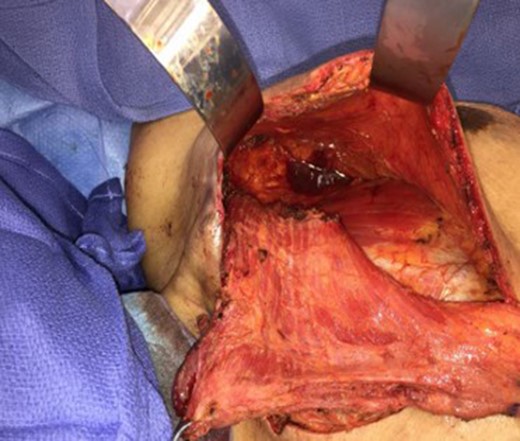
Patient is a 45-year-old female with past medical history significant for paroxysmal atrial fibrillation and diabetes mellitus. She was admitted to the hospital for generalized malaise. She was found to be bacteremic and a CAT scan showed findings consistent with an abscess and resultant osteomyelitis of the left sternoclavicular junction. She underwent multiple debridement by the cardiothoracic team. She had a residual defect at the sternoclavicular joint and a small sized skin defect. She was discharged home with a negative pressure wound therapy device. Patient was readmitted to the hospital with a non-healing wound with active drainage (Fig. 1). These findings were consistent with osteomyelitis and a cutaneous fistula. We recommended further debridement of the wound and bony elements and muscle coverage. Patient was taken to the operating room and Under general anesthesia, the wound was evaluated and marked (Fig. 2). The skin surrounding the cutaneous wound was excised to healthy tissue. The cardiac surgeon assisted in the excision of the non-viable part of the clavicle. At the end of the debridement, the defect included part of the manubrium, most of the medial part of the clavicle and the first rib, the skin overlying the pectoralis in the midline was incised and carried down to the subcutaneous tissue. The ipsilateral pectoralis muscle was dissected and lifted off the chest wall from medial to lateral. The pectoralis was also released inferiorly from it’s attachment to the serratus. The pectoral artery pedicle was identified and preserved. After completely undermining the flap we could not obtain adequate muscle bulk and length to provide adequate coverage. A decision was made to further release the pectoralis from its humeral attachment. The attachment of the pectoralis to the humerus was identified and released (Fig. 3). The result was a completely detached pectoralis except for its attachment at the vascular pedicle (Fig. 4). The muscle was mobilized medially and superiorly to cover the defect. There was adequate coverage for the sternoclavicular defect. Two Jackson Pratt drains, one subcutaneous and the other sub-muscular were placed and secured. The muscle was tacked down with multiple interrupted absorbable sutures. The incision was closed in a layered fashion. Patient tolerated the procedure well. She was discharged home a few days after surgery. The drains were removed in the clinic. Patient was seen for a follow up about 3 months after surgery. The incisions were well healed. She was discharged from the plastic surgery clinic (Fig. 5).




DISCUSSION
Septic arthritis of the sternoclavicular joint is uncommon and presents in about 1% of the general population [1]. There are multiple potential complications of septic arthritis including but not limited to osteomyelitis [2]. In the setting of osteomyelitis, debridement is advocated for source control [3]. Aggressive debridement may lead to bony and soft tissue defects that may need coverage with durable tissue. Soft tissue coverage is imperative for wound healing and cosmesis [3–5].
The use of pectoralis flaps for sternoclavicular joint defect closure have been described in the literature [6]. The pectoralis muscle flaps provide durable tissue for closure and the muscle bulk provide volume to reduce potential contour irregularities. It can be used as an advancement flap base on the thoracoacromial vessels or as turn-over flap bases on the sternal perforators. Recently, Schulman et al. described the use of a hemi islandized pectoralis muscle flap for the reconstruction of a sternoclavicular defect [7]. The use of split pectoralis major flap has also been described [8]. These techniques alleviated the need of detaching the whole flap and preserving the some of the strength of the pectoralis muscle.
Our case illustrates the use of a completely detached pectoralis muscle flap as a technique for sternoclavicular defects with associated non-healing draining fistula. The pectoralis flap can be completely detached from its sternal and humeral attachments and fashioned on a vascular pedicle to obtain adequate length and bulk to allow for a tension free repair of sternoclavicular defects. The patient retained full use of her ipsilateral upper extremity. Although this technique was very successful, It should only be used when the sternoclavicular defect cannot be completely covered after releasing the sternoclavicular attachments as the release of the humeral attachment have been associated with decreased ipsilateral upper extremity weakness.
CONFLICT OF INTEREST STATEMENT
None declared.



