-
PDF
- Split View
-
Views
-
Cite
Cite
Rishabh Sethia, John W Cerne, Kris R Jatana, Charles A Elmaraghy, Pediatric facial kaposiform hemangioendothelioma: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2019, Issue 4, April 2019, rjz113, https://doi.org/10.1093/jscr/rjz113
Close - Share Icon Share
Abstract
Cutaneous kaposiform hemangioendothelioma (KHE) and tufted angioma (TA) are vascular tumors that are often misdiagnosed. Treatment urgency and type varies depending on which tumor-type is diagnosed, because of the differing rates of progression to Kasabach–Merritt phenomenon. An 11-month-old male presented with a facial mass and biopsy results favoring a diagnosis of TA. The diagnosis of KHE, was later favored over TA given the overall clinical picture of initial rapid growth. However, serial imaging showed no subsequent growth, suggesting that clinically diagnosed KHE, may follow a benign clinical course when biopsy results suggest a diagnosis of TA.
INTRODUCTION
Cutaneous kaposiform hemangioendothelioma (KHE) is a vascular tumor with a propensity to cause Kasabach–Merritt phenomenon (KMP). Its prevalence is 0.91 cases per 100 000 children, and the typical presenting location is overlying joints on the extremities [1]. While both on the spectrum of vascular tumors, tufted angiomas (TA) have a more benign growth pattern in contrast to the locally aggressive KHE. KHE will lead to KMP in 70% of cases relative to TA where KMP occurs in about 10% of cases [1–3]. Treatment approach for these tumors is not consistent, largely because cases are so rare and managed by various specialists in different fields. Consensus-derived practice has suggested that managing KHE and TA are based on whether KMP was present. With clinically evident KMP, 64% of centers did not deem a tissue-biopsy necessary to confirm diagnosis. Intravenous vincristine 0.05 mg/kg once weekly AND oral prednisone 2 mg/kg/d OR intravenous methyl-prednisolone 1.6 mg/kg/d was recommended. Without clinical evidence of KMP, oral prednisolone 2 mg/kg/d is recommended with the consideration of adjunctive aspirin 2–5 mg/kg/d [4]. Treatment guidance, however, is not defined for when KMP is not present but appears imminent.
CASE REPORT
An 11-month-old male with a history of nasolacrimal duct stenosis and 4 mm thyroglossal duct cyst presented for evaluation of left facial swelling for 9 months. Approximately 6 months prior to admission, a mass was identified on the left cheek which had progressively increased in size over the past 2 months. The patient also had intermittent fevers the week prior to admission but was otherwise healthy. Baseline labs, including platelets, were within normal limits. On exam, he was found to have a firm, mobile, non-tender mass just inferior to the left zygomatic arch. Ultrasound revealed a vascularized solid lesion measuring 12 mm × 15 mm × 16 mm limited to the superficial soft tissues. MRI showed a multi-lobular mass with increased T2 signal centered within the left masseter and infiltrating signal in surrounding subcutaneous tissue (Fig. 1). The patient subsequently underwent ultrasound-guided core biopsy. The initial pathological diagnosis was consistent with TA, showing fibrovascular tissue containing compact nests of variably sized and ill-defined vascular channels. Immunohistochemistry staining showed the endothelial cells to be diffusively reactive for CD34 and CD31, partially reactive for D2-40, and negative for GLUT-1. However, upon further review, KHE was favored given the solid and infiltrative components on MRI, normal overlying skin on exam, and location of the lesion within subcutaneous fat. Accordingly, low-dose daily aspirin was prescribed prophylactically to prevent KMP. An MRI 2 months later, along with serial ultrasound images in the ensuing 26 months, showed no further growth (Fig. 2). His parents noted intermittent painless changes in size that did not seem to be related to any stimulus and returned to baseline size within hours. Surgical intervention at 3 years old is anticipated.
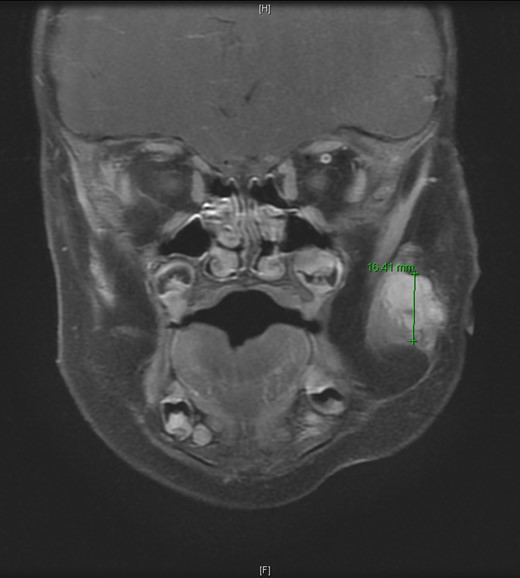
T2-weighted MRI revealed a homogenously enhancing 13 mm × 11 mm × 16.4 mm mass with indistinct margins centered within the left masseter muscle and protruding into the subcutaneous tissues laterally.
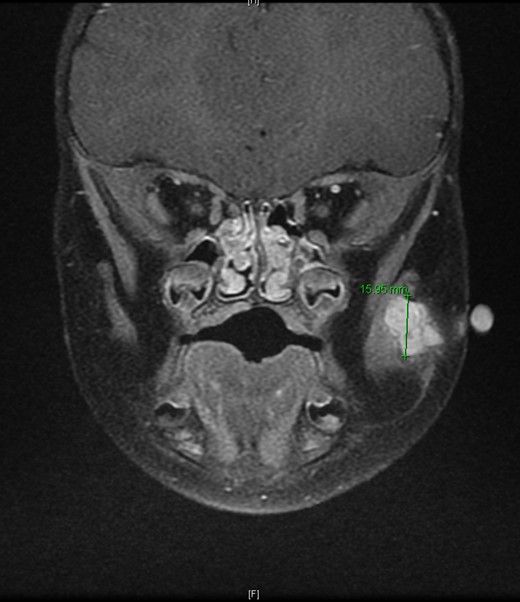
T2-weighted MRI 2 months later revealed a 14.5 mm × 14.1 mm × 15.95 mm mass partially involving the masseter muscle with no internal vascular flow voids.
DISCUSSION
KHE rarely presents in the cervicofacial region. This case illustrates the clinical course of this rare presentation. The D2-40 immunohistochemistry staining pattern of the biopsy specimen, along with other tissue characteristics, did not definitively rule out KHE but did indicate TA as being the more likely diagnosis. The staining pattern of D2-40 has been suggested as a useful method for distinguishing KHE from TA [5]. Properties of the tumor on MRI imaging, being located in the deep dermis, deep tissues, subcutis, and muscle as opposed to dermis and superficial subcutis supported the diagnosis of KHE [6].
Rapid growth was expected to continue after the time of diagnosis, as this is what occurred in the preceding 2 months. Though TA was initially favored due to the biopsy results, the overall clinical picture led to a diagnosis of KHE and the prescription of low-dose aspirin. In conversations with the patient’s family at visits, it was discovered that aspirin was not being given to the patient. In retrospect, this was fortuitous because no further growth was observed, and no signs of KMP appeared. Platelet counts provide an early clue to the development of coagulopathy; the fact that baseline platelet values were within normal limits may have warranted further consideration in deciding upon this patient’s treatment approach [7].
Though typically appearing on extremities, KHE and TA should always be considered in the differential for an infantile facial mass. This patient’s clinical course suggests that KHE has a low propensity for KMP and clinical progression when biopsy results support a diagnosis of TA, rather than KHE. Given the importance of factoring in concern for Reye’s syndrome, low-dose aspirin may not be warranted when biopsy results support a diagnosis of TA. Consensus-derived opinion supports this, stating that low-dose aspirin should be considered in such patients, only when presenting with complications from expansion. This case illustrates that ‘active nonintervention’ with close surveillance is a reasonable approach. While this approach has been supported in treating uncomplicated cases, it has not been recommended for cases that seem likely to become complicated [6].
CONFLICT OF INTEREST STATEMENT
None declared.



