-
PDF
- Split View
-
Views
-
Cite
Cite
Samer Kawak, Hassan Turaihi, Paul Bjordahl, Transanal stricturoplasty: a minimally-invasive approach to a challenging problem, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz087, https://doi.org/10.1093/jscr/rjz087
Close - Share Icon Share
Abstract
Despite the advances in the surgical techniques and technology in colorectal surgery, the development of rectal anastomotic stricture is a common problem. In some case series, the incidence is estimated to be as high as 30%. Some of the known risk factors for developing a stricture include anastomotic leak and ischemia. Treatment options range from frequent dilations using digital rectal examinations and dilators if the stricture is low or endoscopic balloon dilations for higher strictures. Unfortunately, multiple sessions are typically required to achieve adequate results. We present a case report of a benign anastomotic stricture and describe a novel approach, transanal stricturoplasty, for this challenging problem.
INTRODUCTION
Stricturoplasty is a surgical procedure performed to relieve bowel strictures commonly caused by inflammatory bowel disease. Repeat episodes of inflammation lead to continued fibrosis and scar formation and eventual stricture formation. With these strictures, a narrowing of the bowel is noted, and the potential of a lead point obstruction is present. The purpose of stricturoplasty is to dilate these narrowing without the need to remove bowel segments [1]. In rectal anastomotic strictures, a transanal stricturoplasty is a possible treatment modality.
CASE REPORT
The patient is a 55-year-old female who presented to the emergency department with stabbing lower abdominal pain. Her examination revealed focal peritonitis in the left lower abdomen. Patient’s laboratory testing was remarkable for a leukocytosis. Computed tomography demonstrated left-sided uncomplicated acute diverticulitis. The patient was admitted for medical management with intravenous antibiotics and bowel rest. On hospital Day 3, she continued to complain of severe pain and was subsequently offered surgical intervention. She underwent a sigmoid resection with end colostomy, and after an uneventful postoperative course she was discharged home.
Three months after her initial surgery, the patient presented to the office requesting a colostomy reversal. An outpatient colonoscopy showed mild diverticulosis but was otherwise unremarkable. She underwent a laparoscopic colostomy reversal using a 28-mm end-to-end anastomosis (EEA) stapler. Again, her postoperative course was unremarkable, and at the time of discharge she was tolerating a regular diet and had appropriate bowel function.
The patient presented to her gastroenterologist 1 year after her colostomy reversal with constipation associated with diffuse abdominal pain and bloating. There was no report of weight loss or hematochezia. A colonoscopy was performed that revealed a near-complete stenosis of the rectal anastomosis. The patient was referred back to our clinic to discuss surgical options. Due to her favorable anatomy and the benign nature of her pathology, she was offered an open or laparoscopic stricturoplasty, endoscopic balloon dilation, or endoscopic transanal stricturoplasty. She elected to proceed with the latter after the risks and benefits of the procedure were explained.
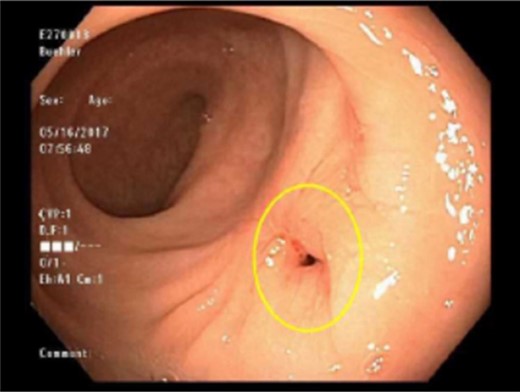
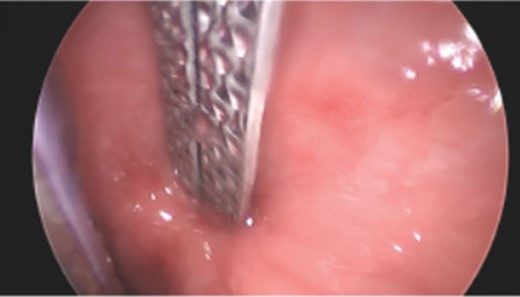
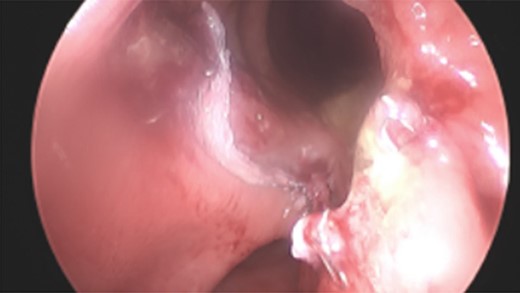
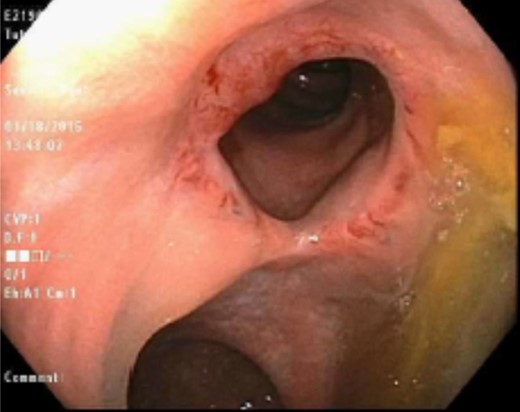
After informed consent was obtained, the patient was brought to the operating room and positioned in the lithotomy position. A urinary catheter was inserted, and preoperative IV antibiotics were administered. A single-site transanal gelport (GelPOINT® Path Transanal Access Platform by Applied Medical) was positioned transanally. Low pressure pneumorectum was achieved and 0° bariatric scope was introduced through the anus into the rectum. The previous anastomosis was noted to be 15 cm from the anal verge and was clearly stenotic (Fig. 1). Following gentle spreading of the stricture, a 60-mm purple load Endo GIA stapler was advanced under direct visualization across the anastomosis where one blade was position across the afferent limb and the other blade was positioned in the blind pouch (Fig. 2). Firing the stapler led to the creation of a widely patent anastomosis (Fig. 3). The patient was admitted to the general ward for observation. She was discharged the next day after tolerating a regular diet. Four weeks postoperatively, she reported completed resolution of her symptoms. She underwent a surveillance colonoscopy 6 months after the stricturoplasty, and a widely patient anastomosis was still observed (Fig. 4).
DISCUSSION
Colorectal anastomotic strictures are not an uncommon occurrence [2]. A colorectal stricture causing a small bowel obstruction is characterized by an inability to pass a 12-mm proctoscope or a 19-mm rigid sigmoidoscope through the stenosis [3, 4]. There are several possible etiologies to these strictures including prior resections, endoscopic submucosal dissection, colostomies, and radiation.
The clinical manifestation of a colorectal stricture depends on the location and stenosis severity. The most common presentation is altered bowel habits [5, 6]. In obstructive cases, patients have no signs of bowel function and may have localized pain. The risk of bowel perforation is imminent, especially if no timely intervention is performed. Management of strictures depends on the patient’s clinical status at that time of presentation. The main etiology and location of the stricture are necessary to consider prior to any intervention.
In cases where a malignant process was previously present, the risk of recurrence should be fully investigated. A tissue biopsy should be obtained from the area of concern prior to any intervention on the stricture. Distal benign strictures (within 10 cm of the anal verge) can be effectively treated with frequent dilations. More proximal benign strictures can be treated with endoscopic balloon dilation [3, 4]. Endoscopic dilation requires the ability to pass a guidewire through the narrowed segment of the colon under fluoroscopic guidance. There is very minimal morbidity associated with this procedure [7]. In a study by Suchan et al., 94 patients with colorectal anastomotic strictures were analyzed. Endoscopic dilation was found to be more successful in the benign stricture group compared to the malignant one. Complications of endoscopic dilation include restenosis, perforation, and abscess formation [4].
A metallic stent is another option available for anastomotic strictures. A stent can be used in conjunction with dilation to maintain patency, especially if the latter is unsuccessful. The conventional surgical approach entails complete resection and revision of the anastomosis, which is associated with a higher morbidity and mortality. In this case report, a transanal stricturoplasty was performed as the definitive intervention. This approach is safe and as effective as conventional methods in patients with favorable anatomy [8].
Acknowledgments
None.
CONFLICT OF INTEREST STATEMENT
None declared.



