-
PDF
- Split View
-
Views
-
Cite
Cite
Enver H Fekaj, Concomitant necrobiosis lipoidica and splenic abscess, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz088, https://doi.org/10.1093/jscr/rjz088
Close - Share Icon Share
Abstract
Necrobiosis lipoidica is an idiopathic dermatosis of unknown origin, occurring mainly in patients with diabetes. Splenic abscesses are rare entities. We report a case with concomitant necrobiosis lipoidica and splenic abscess. A 58-year-old man presented to emergency center with a two day history of left upper abdominal pain, general malaise, and pyrexia. On both lower legs the patient had skin lesions. The contrast-enhanced computed tomography of the abdomen revealed splenomegaly and splenic abscess in the upper pole of the spleen. On the fourth day after admission, patient underwent open splenectomy. For the lesions on lower legs, by clinical examination, necrobiosis lipoidica was confirmed. The patient was treated by topical administration of steroid cream. After a 2 months follow-up, this treatment was not effective. Left upper abdominal pain and pyrexia in patient with necrobiosis lipoidica may suggest splenic abscess.
INTRODUCTION
Necrobiosis lipoidica (NL) is an idiopathic dermatosis of unknown origin, occurring mainly in patients with diabetes. Its incidence ranges from 0.3% to 1.6% in patients with diabetes mellitus per year, and mainly affecting the women. The lesions are usually observed on both lower legs. Diagnosis is made by clinical examination. Histopathological examination may be required in early stage of the disease or in nondiabetic patients [1].
Splenic abscesses commonly occur in the patients with hematologic disorders, diabetes, endocarditis, acquired immunodeficiency syndrome (AIDS), and urogenital infections [2]. Traditionally, antibiotics and splenectomy were considered as the treatment of choice. In some patients, spleen-preserving management with percutaneous image-guided drainage is favored [3]. We aimed to report a rare case with concomitant necrobiosis lipoidica and splenic abscess in patient with diabetes.
CASE REPORT
A 58-year old man presented to our emergency center with a 2-day history of abdominal pain in the left hypochondrium, general malaise and pyrexia. The physical examination of the abdomen was normal. On both lower legs, the patient had yellow-brown skin lesions with indurated borders (Fig. 1). On the right leg this lesion was located on the pretibial area (Fig. 2), while on the left leg the lesion was located in the medial part of crural region.

Necrobiosis lipoidica: Yellow-brown skin lesions with indurated borders located on both lower legs.

The lesion (necrobiosis lipoidica) on the right lower leg located on the pretibial area.
At the admission, erythrocyte sedimentation was 80 mm/h (normal value 3 mm/h), C-reactive protein was 137.7 mg/l (normal value 0.0–6.0 mg/l), leukocytes were 14.2 × 103/μL (normal value 4.0–10.0 × 103/μl), and glycaemia was 14.81 mmol/l (normal value 4.40–6 mmol/l), while other biochemical parameters were normal. The CECT of the abdomen revealed splenomegaly and splenic abscess in the upper pole of the spleen (Fig. 3). No abscesses elsewhere in the body were detected. Systemic hematologic disorders are excluded. Initially, the patient was treated by imipenem- cilastatine. After the admission, on the fourth day, patient underwent open splenectomy. Enterococcus faecalis has been isolated from splenic abscess. On the seventh postoperative day the patient was discharged. The patient was in very good condition a month later after splenectomy. For the lesions on lower legs, based on clinical examination, necrobiosis lipoidica as a diagnosis was confirmed. The disease was in later stage and histopathologic examination was not necessary. This patient was treated by topical administration of steroid cream (Exevate cream 0.05%). After a 2 months follow-up, this treatment was not effective, but continuous to be under surveillance of dermatologists.
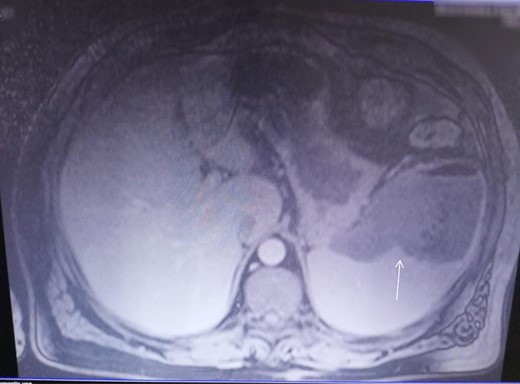
CECT investigation revealed abscess and air presence in the upper pole of the spleen.
DISCUSSION
Necrobiosis lipoidica diabeticorum (NLD) occurs in 0.3–1.6% of diabetic patients with a predisposition for affecting women and those who are insulin dependent [4].
The lesions of NLD start in the pretibial areas with characteristic erythematous papules that gradually enlarge and converge into large plaques, with yellow pigmentation at the center and red-brown or violaceous pigmentation at the periphery. On the later stage of the disease, the center of the lesion may become atrophic with superficial teleangiectasias [1, 4].
In most cases, diagnosis is made by clinical examination, although, some diseases such as sarcoidosis, granuloma annulare, and lichen sclerosus et atrophicus may be differential diagnosis of NLD [1]. In our patient, diagnosis was made by clinical examination.
Actually, treatment of NLD mostly includes intralesional administration of triamcinolone, short courses of systemic steroids, topical administration of steroids, acetylsalicylic acid, dipyridamole, pentoxyphilline, fibrinolytic therapy, and chloroquine [1, 5, 6]. Our patient was treated by topical administration of corticosteroid cream (Exevate cream 0.05%). After a 2 months follow-up, this treatment was not effective.
The most common causes of splenic abscesses are abdominal infections, diabetes, pneumonia, bacterial endocarditis, urogenital infections, and some hemoglobinopathies [3]. Splenic abscess can be developed in patients with acute brucellosis, although this is a rare event [7].
In a patient with pyrexia of unknown origin, left hypochondriac pain, leukocytosis, and splenomegaly splenic abscess should always be suspected [3]. Our patient presented with a 2-day history of abdominal pain in the left hypochondrium, general malaise, and pyrexia, and with erythrocyte sedimentation, C-reactive protein and leukocytes highly elevated. The CECT imaging of the abdomen revealed splenomegaly and splenic abscess in the upper pole of the spleen.
The management of splenic abscess is based on medical therapy with antibiotics, and splenectomy or percutaneous drainage (PCD). Ultrasound-guided or CT-guided percutaneous drainage is advised for unilocular or bilocular abscesses, and for the patients who are critically ill. For multiple abscesses is reported that splenectomy is a safe and effective treatment choice [3, 8].
The recommendation is that treatment should be tailored on an individual basis [8]. Our patient underwent open splenectomy.
To our knowledge, this is the first case in literature presenting concomitant necrobiosis lipoidica and splenic abscess.
In conclusion, left upper abdominal pain, pyrexia, and leukocytosis in patient with necrobiosis lipoidica may suggest splenic abscess. Clinical, biochemical, and imaging examinations are needed for further evaluation and appropriate treatment. Treatment modality should be tailored on an individual basis.
Acknowledgments
The author declares that he has no acknowledgments.
CONFLICT OF INTEREST STATEMENT
None declared.
Funding
None.



