-
PDF
- Split View
-
Views
-
Cite
Cite
Catarina Morais, Ezequiel Silva, Pedro Nuno Brandão, Raquel Correia, Susan Foreid, Vítor Valente, Neuroendocrine tumor of the appendix—a case report and review of the literature, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz086, https://doi.org/10.1093/jscr/rjz086
Close - Share Icon Share
Abstract
Incidental appendiceal neuroendocrine tumors (ANETs) occur in 0.2–0.7% of surgical resections for suspected appendicitis (Moris, Tsilimigras, Vagios, Ntanasis-stathopoulos, Karachaliou, Papalampros, et al. Neuroendocrine neoplasms of the appendix: a review of the literature. Anticancer Res [Internet]. 2018;38:601–11.). It’s a rare entity, clinically challenging and has controversy surrounding its management. A 69-year-old male presented to our clinic with acute right lower quadrant abdominal pain with less than 24 hours of evolution. The presumed clinical diagnosis was acute appendicitis. It was performed a laparoscopic appendectomy and the histopathologic result of the specimen showed neuroendocrine tumor of the appendix. ANETs are rare and typically diagnosed as incidental histopathologic finds in appendices specimens. However, they are the most common tumors arising from de appendix, between 30% and 80% of the cases (Pape, Niederle, Costa, Gross, Kelestimur, Kianmanesh, et al. ENETS consensus guidelines for neuroendocrine neoplasms of the appendix (excluding goblet cell carcinomas). Neuroendocrinology. 2016;103:144–52). Appendectomy may be sufficing for tumors <2 cm and they are associated with good long-term outcomes.
INTRODUCTION
Neuroendocrine tumors (NETs), which were first described by Oberndorfer in 1907, arise from enterochromaffin cells found throughout the gastrointestinal tract and the broncho-pulmonary system. ANETs are the third most frequent (16.7%) gastrointestinal neuroendocrine tumors, with the small bowel (44.7%) and the rectum (19.6%) occupying the first and second positions, respectively [1].
There seems to be a slight female predominance for ANETs. In contrast to other appendiceal tumors and other NETs, which tend to occur in older patients, ANETs show highest incidence rates at 15–19 years of age in women and 20–29 years in men. The mean age of patients in the latest study by Pawa et al. was 33.2 (range = 7–79) years, with a female predominance (60.5%) [2].
Most ANETs are found incidentally in histopathologic exam of appendices specimens for presumed acute appendicitis [3].
ANET carry better survival rates (>95%) compared to all other tumor types located in the appendix, even patients with locoregional disease seem to have approximately the same prognosis as those having tumors limited to the appendix [4].
Current guidelines suggest that simple appendectomy is adequate treatment for ANETs if they are <1 cm, and right hemicolectomy is recommended for those bigger than 2 cm. However, ideal treatment of 1–2 cm tumors is still controversial [5, 6].
Despite their indolent course, some ANETs may relapse. Resected tumors >2 cm or >1 cm with additional risk factors need to be followed for at least 7 years.
CASE REPORT
A 69-year-old male patient, with no relevant past medical history, was admitted to University Hospital Center of Oporto (Oporto, Portugal) with acute right lower quadrant abdominal pain with less than 24 hours of evolution. No other symptoms associated.
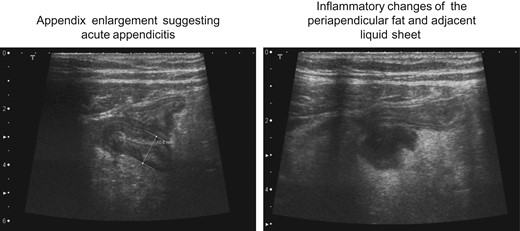
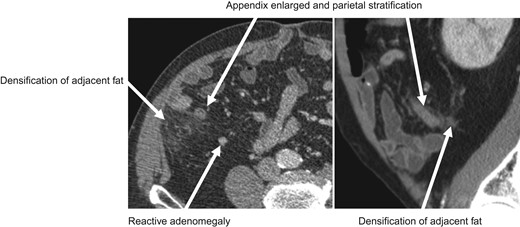
At physical examination, the patient was distressed, with body temperature of 37°C, hemodynamically stable, no signs of respiratory distress. The abdominal examination revealed the presence of positive Rovsing and Blumberg signs and no palpable masses. Laboratory tests were performed, yielding the following results: white blood cell count, 10.3 × 10^3cells/μL; neutrophil proportion, 77.2%; hemoglobin level, 14.4 g/dl; platelet count 149 × 10^3cells/μl; C-reactive protein 32.77 mg/l; sodium 141 mmol/l; creatinine 1.06 mg/dl. Without changes in the coagulation study. Abdominal ultrasound (Fig. 1) and CT scan (Fig. 2) revealed the findings consistent with appendicitis.
The patient underwent to a laparoscopic appendectomy. Intraoperatively, an acute suppurative appendicitis with localized abscess was diagnosed. The resection of the appendix was completed. The patient completed antibiotherapy course and was discharged 5 days after, with no complications.
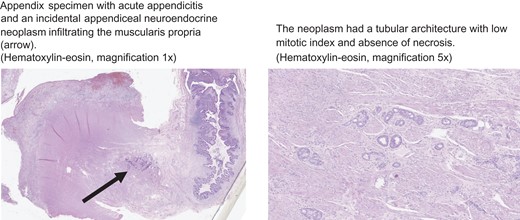
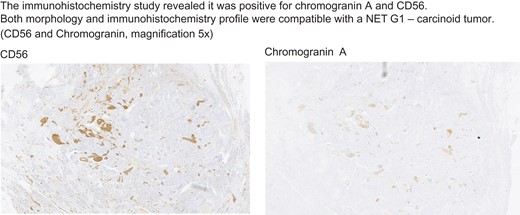
The histopathological exam of the specimen showed acute appendicitis with morphologic aspects and immunohistochemistry (chromogranin A and CD56 +) well matched with neuroendocrine tumor of the appendiceal tip (pT1R0-G1), (Figs 3 and 4), measuring 6 mm at the maximum dimension, infiltrating the muscular layer. The mitotic activity of the lesion was low (<2 mitosis/10× magnification). Coexisting acute suppurative appendicitis was also present.
The case was discussed in a multidisciplinary oncologic reunion and was decided for surveillance.
DISCUSSION
Although not a common entity, neuroendocrine tumors of the appendix should be considered as a cause of acute appendicitis during appendectomy and since, in our institution, we send all de appendix specimens to histopathological examination, we are able to identify incidentally some cases of ANETs. Classic carcinoid syndrome (flushing, diarrhea and cardiac disease) is very uncommon (<1%) [7] and more likely to appear in patients whit advanced disease.
NETs are identified in numerous locations, including the lung (25.1%), ovaries (0.5%), biliary system (0.2%) and gastrointestinal tract (73.4%) [8] and ANETs are located most commonly at the tip of the appendix—75% of cases, at the base of the appendix in 5%, and in the mid-section in 20% [9], with a mean tumor size about 6 mm (range 0.4–14 mm) [5]. The histopathological diagnosis of NETs includes determination of the immunohistochemistry profile of the tumor in regard to synaptophysin and chromogranin A (CgA), as well as the proliferative marker, the Ki-67 index [5].
According to the current WHO (World Health Organization) and ENETS (European Neuroendocrine Tumor Society) grading systems, NET-G1 is labeled by a mitotic count of <2 per 2 mm2 (40× magnification) and Ki-67 ≤2%; NET-G2 by a mitotic count of 2–20 per 2 mm2 or Ki-67 of 3–20%; NET-G3 by mitotic count of >20 per 2 mm2 or Ki-67 index >20%. Many parameters have to be taken into account for the distinction of tumors with a mild clinical course from those with a more aggressive potential carrying a higher risk for locoregional relapse and distant metastasis, including the tumor size and its exact location, the extent of infiltration of the appendix wall or possible vascular invasion and the proliferative rate [1].
ENETS guidelines suggest that long-term follow-up, and not completely evidence-proven, only when lymph node involvement is present, locoregional disease is identified postoperatively and when the tumor is of high stage. Regular monitoring is necessary for patients with tumors sized between 1 and 2 cm with features indicating a higher risk for lymph node dissemination of the disease, such as mesoappendiceal invasion >3 mm, localization in the base of the appendix, vascular infiltration or intermediate differentiation (G2) [1]. Furthermore, follow-up is also not mandatory for tumors larger than 1 cm for which right hemicolectomy was performed and if no additional risk factors were present such as lymphovascular invasion [2].
In this clinical case, the tumor was located at the tip of the appendix and the patient experienced acute right lower abdominal pain witch lead to the clinic diagnosis of acute appendicitis. The surgical procedure was performed for the treatment of appendicitis, and the NET was identified incidentally during the histological examination. In the present patient, the tumor was 0.6 cm in diameter and therefore, in the light of current knowledge of ANETs treatment, no additional treatment was needed.
Follow-up of small tumors (<1 cm) treated with appendectomy and excised in clear margins (R0) is not suggested by the ENETS guidelines [5].
SEER (Surveillance, Epidemiology, and End Results) database studies report 5-year survival rates of 94% for confined lesions, 84.6% for locoregional disease and 33.7% when distant metastasis are present [8, 10].
CONFLICT OF INTEREST STATEMENT
None declared.



