-
PDF
- Split View
-
Views
-
Cite
Cite
Ryohei Ushioda, Hiroto Kitahara, Hayato Ise, Yuta Koichi, Naohiro Wakabayashi, Chiharu Tanaka, Sentaro Nakanishi, Natsuya Ishikawa, Hiroyuki Kamiya, A case of pulmonary artery sarcoma that was initially mis-diagnosed as pulmonary embolism, Journal of Surgical Case Reports, Volume 2019, Issue 3, March 2019, rjz078, https://doi.org/10.1093/jscr/rjz078
Close - Share Icon Share
Abstract
Pulmonary artery sarcoma is a rare and highly malignant neoplasm. Early diagnosis and a multidisciplinary approach including surgical treatment and optimal medical therapy could prolong survival. Since the clinical symptoms and imaging findings of pulmonary artery sarcoma mimic pulmonary embolism, definitive diagnosis and surgical intervention are often delayed. In this report, a case of pulmonary artery sarcoma that was initially misdiagnosed as pulmonary embolism is presented.
INTRODUCTION
Pulmonary artery sarcoma (PAS) is a rare, highly malignant, mesenchymal tumor. The clinical presentation in patients with PAS is very similar to that with pulmonary embolism (PE), and, therefore, it is frequently misdiagnosed as acute or chronic PE. PAS should be considered in patients with suspected PE, especially that which is refractory to anticoagulant therapy. A case of PAS that was initially misdiagnosed as PE is presented.
CASE REPORT
A 60-year-old man presenting with acute onset dyspnea and chest pain was referred to our institution. He had no past medical history. Physical examination was essentially normal except for weak respiratory sounds on the right side. Oxygen saturation was 88%. D-dimer was 1.43 mg/l. The electrocardiogram showed no ST changes. Chest radiography showed an abnormal shadow in the hilum of the right lung. Color Doppler ultrasound showed no deep vein thrombosis. Both the Wells Score and the Revised Geneva Score were 0. Transthoracic echocardiography showed normal left ventricular function (ejection fraction 62%), and no findings of pulmonary hypertension. Contrast-enhanced computed tomography (CT) showed a contrast defect lesion in the right and main pulmonary arteries, as well as a right pleural effusion (Fig. 1). He was initially diagnosed with PE according to the imaging findings and clinical presentation. Anticoagulant therapy (intravenous heparin infusion) was then started. Follow-up CT showed a larger defect lesion in the pulmonary artery, and the decision was then made to proceed with urgent pulmonary embolectomy because it was refractory to anticoagulant therapy. Cardiopulmonary bypass was established with aortic and bicaval cannulation. Deep hypothermic circulatory arrest was used every 10 minutes to obtain a bloodless field during pulmonary embolectomy. The right pulmonary artery was incised, and it was filled with a red, solid mass (Fig. 2). The mass was resected, and the pathological diagnosis during surgery was PAS. Because of the urgent situation, only endarterectomy, not pneumonectomy for radical resection of the tumor, was performed. On postoperative Day 7, CT showed residual lesions in the right pulmonary artery. The pathology report showed high-grade undifferentiated PAS (Fig. 3). The patient refused radical tumor resection by pneumonectomy, as well as postoperative radiation and chemotherapy. He died 5 months after the surgery.
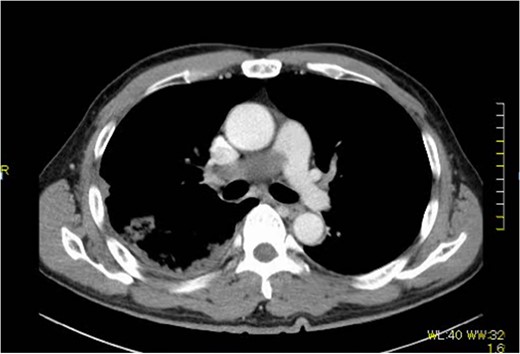
Extensive contrast-deficient images ae present from the pulmonary artery trunk to the right pulmonary artery.

Macro findings of the pulmonary artery show sarcoma and thrombus.
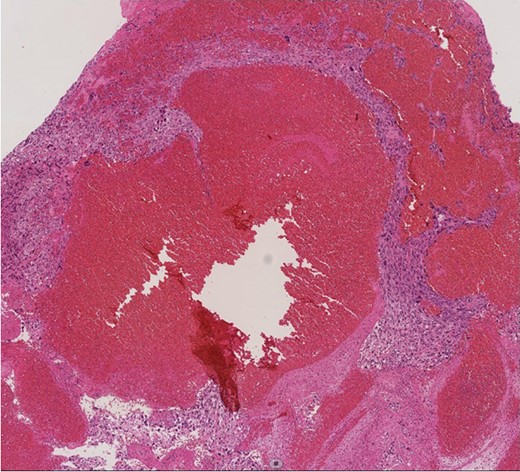
Histopathological image (×100). Histologic analysis of the specimen shows high-grade undifferentiated sarcoma due to polymorphism with mitoses and a polychromatic inner lining. Necrotic tissue and thrombi are also present in the tumor, with invasion into the fibrous intima of the pulmonary artery.
DISCUSSION
Less than 400 PAS cases have been reported since it was first described by Mandelstamm in 1923 [1]. PAS has a very poor prognosis, and survival time is reported to be as short as 1.5 months without surgical treatment [2]. Early diagnosis and surgical intervention are very important. Several authors reported that surgical resection was effective for alleviating symptoms and prolonging survival time in patients with PAS [3, 4]. The diagnosis of PAS is sometimes challenging because the clinical presentation and imaging findings are similar to those of PE. Therefore, PAS is frequently misdiagnosed as acute or chronic PE, which delays surgical treatment in many cases. In the report of Bandyopadhyay, nearly half (47%) of the patients with PAS were originally misdiagnosed as having PE, including 39% who received thrombolytic and/or anticoagulant therapy [5]. A definitive diagnosis can be made only by biopsy or surgery. However, biopsy procedures (percutaneous, transbronchial, or intravenous) are invasive and not routinely performed. A preoperative diagnosis of PAS is established by a multidisciplinary approach based on contrast-enhanced CT, MRI, PET-CT, and transesophageal echocardiography (TEE). On CT, PAS is seen as a large, cauliflower-like, nonuniform contrast effect, and it is relatively often seen in the central part of the pulmonary artery [6]. On MRI, PAS shows a medium to low signal on T1W, a high signal on T2W, and a heterogeneous enhancement effect [7]. TEE is a helpful tool that is able to identify planar invasion of the tumor into the arterial wall. Ito et al. reported that PET-CT was able to differentiate PAS and PE by the SUV max value (7.63 ± 2.21 in PAS, 2.31 ± 0.41 in PE) [8]. However, with the imaging findings, only 36% of patients were diagnosed with PAS before the biopsy result or surgical intervention [5]. The present case was resistant to anticoagulant therapy, and the test scores suggesting the probability of PE were low (Wells score: 0, Revised Geneva Score: 0). The patient was scheduled for PET-CT or MRI for further diagnostic work-up, but he needed urgent surgery because of tumor growth on CT before that could be done. The surgical options for PAS include either pneumonectomy or pulmonary endarterectomy, which was reported to be effective for achieving symptom relief and prolonging survival in patients with PAS [9, 10]. As noted by Grazioli et al., patients who underwent pneumonectomy had a better survival rate than those who underwent pulmonary endarterectomy. However, if pulmonary hypertension was present or the tumor was bilateral, pneumonectomy did not improve survival. Therefore, in such cases, pulmonary endarterectomy was recommended as a palliative treatment [9]. In the present case, neither finding was seen, and therefore pneumonectomy was recommended. However, the family and the patient did not want radical treatment because of the risk and the hospital stay. Thus, only pulmonary endarterectomy was performed. In conclusion, early diagnosis and complete surgical resection offer the best chance for prolonged survival for patients with PAS. However, depending on the patient’s condition, palliative pulmonary endarterectomy could be considered an option.
CONFLICT OF INTEREST STATEMENT
None declared.



