-
PDF
- Split View
-
Views
-
Cite
Cite
Mirza M A S Baig, Rikesh Patel, Mohamad Ali Kazem, Arif Khan, Schwannoma in the ascending colon, a rare finding on surveillance colonoscopy, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz046, https://doi.org/10.1093/jscr/rjz046
Close - Share Icon Share
Abstract
Schwannomas are peripheral nerve sheath tumours that can present as a rare tumour of GI tract, and even more uncommonly within the colon. We present a case of colonic schwannoma in an asymptomatic patient identified on surveillance colonoscopy. The tumour is of mesenchymal origin and is often challenging to diagnose prior to surgical resection. Endoscopy usually fails to provide adequate sample and diagnosis is usually confirmed on immunohistochemistry.
INTRODUCTION
Schwannomas of the gastrointestinal tract are spindle cell tumours that originate from peripheral nerve lining Schwann cells. Outside the central nervous system it represents a rare entity, accounting for approximately 2–6% of all mesenchymal tumours [1]. As it normally arises from intracranial nerves and spinal nerves, neurosurgeons encounter the bulk of these cases, however surgeons, radiologists, gastroenterologists and histopathologists are occasionally consulted. These tumours present a diagnostic challenge radiologically and endoscopically, as mucosal biopsies are inadequate to differentiate them from other GI tumours. Immunohistochemistry is the source of diagnosis [2, 3].
Schwannomas are generally benign, slow growing with a very low malignant potential [1, 4]. The stomach is the most commonly affected region of the GI tract (83%) followed by small bowel (12%) and colon/ rectum [5].
CASE PRESENTATION
We present the case of a 75-year-old female patient, previously fit and well, who presented with the extremely rare finding of an ascending colon schwannoma. She was already under surveillance colonoscopy by the gastroenterologists because of her strong family history of bowel cancer.
Previous colonoscopy, 4 years prior, had found several benign polyps. On recent colonoscopy, a 2 cm submucosal lesion within the ascending colon was identified and thought to be a lipoma (Figure Xa and Xb). Biopsies taken at the time were found to be benign with only oedematous large bowel mucosa seen, however these were superficial and no submucosal tissue was present (Figs 1–7).
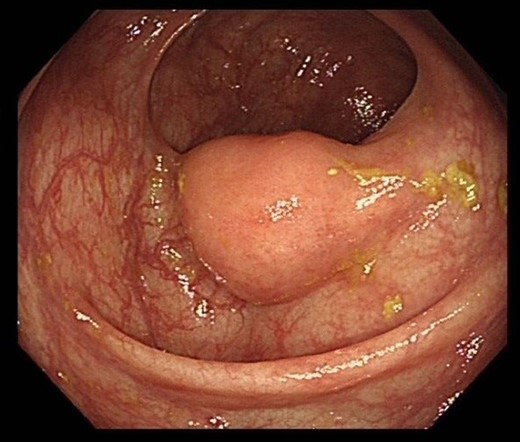
Colonoscopy image of the ascending colon showing submucosal lesion.
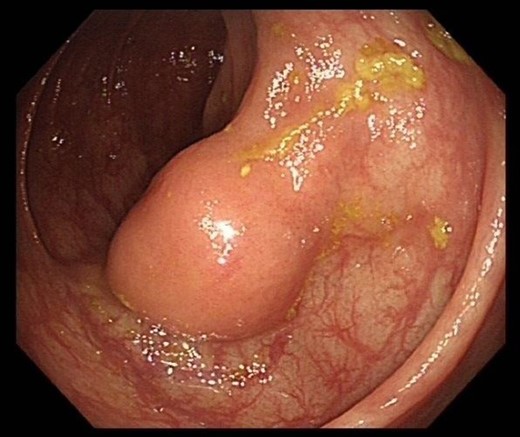
Colonoscopy image of the ascending colon showing submucosal lesion.
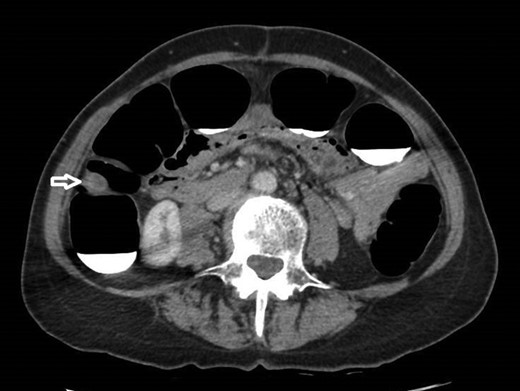
12 mm polypoidal mass (white arrow) visible on axial image of post-contrast CTVC.

12 mm polypoidal mass (white arrow) visible on coronal image of post-contrast CTVC.

12 mm polypoidal mass (white arrow) visible on sagittal image of post-contrast CTVC.
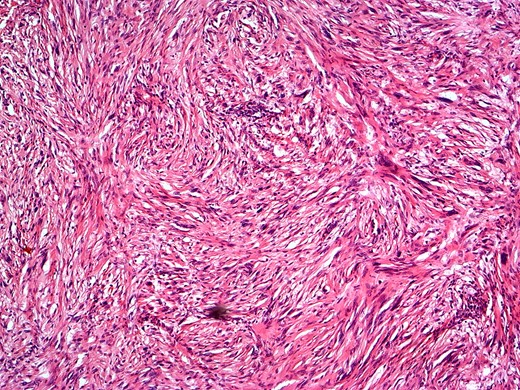
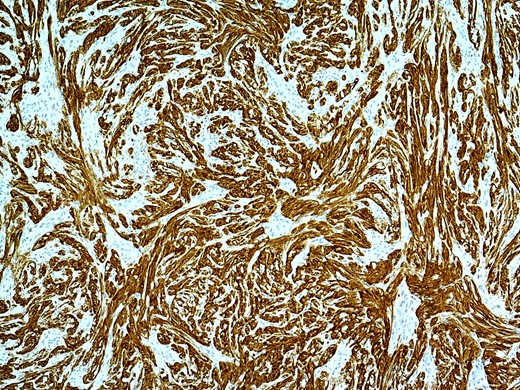
H&E staining showing submucosal tumour with spindle cells and verocay bodies.
In view of this CT Colonoscopy was performed, alongside a CT Chest examination. This showed a 12 mm lesion arising from the lateral wall of the ascending colon. It appeared rounded and mural-based, and displayed irregular peripheral enhancement post-contrast. It did not conform with a lipomatous lesion, with an average internal density of approximately 40 HU. No other colonic lesions were demonstrated, and no locoregional adenopathy or distant metastases were identified.
Based on the endoscopic and radiological findings, the differential diagnoses included the other rare causes of submucosal tumours like GIST, GI autonomic neural tumour, leiomyoma, leiomyosarcoma, lymphoma, schwannoma and metastatic melanoma.
The case was discussed at the MDT and the multidisciplinary team felt that this was not a lipoma and warranted excision. The patient underwent an uncomplicated laparoscopic right hemicolectomy with an uneventful post operative course and was discharged on Day 6.
Macroscopically, there was a bump on the lateral wall close to the distal resection margin. The bump was firm to the touch.
Microscopically, there was an unencapsulated, round tumour centred on the submucosa and muscularis propria. The tumour was composed of fascicles of spindle cells, including some palisading of nuclei (Verocay bodies), however, no significant atypia and no mitoses are seen. The tumour was strongly positive for S100. A diagnosis of Schwannoma was made.
As the postoperative histology showed complete resection and benign pathology, no further treatment was required. These tumours are noted to have a good prognosis.
The patient visited the clinic after four weeks and had recovered well. She was informed of the reassuring histopathology report and was advised to follow her surveillance colonoscopies as before.
DISCUSSION
Schwannomas are extremely rare tumours of nerve sheaths, developing from Schwann cells. In the GI tract, they present as spindle cell tumours and account for approximately 2–6% of all mesenchymal tumours [1].
Colorectal schwannoma is a rare GI neoplasm and is the least frequent location for a GI schwannoma [5], stomach being the most common [6]. It has a slightly higher female predominance [59%] and usually present in the sixth decade [7]. There are currently only 95 cases reported in the literature, of which 29 were within the caecum and the ascending colon [2]. They are mostly discovered on screening colonoscopies or CT scans for other reasons, as the majority are asymptomatic. Occasionally symptoms include rectal bleeding, abdominal pain, constipation and tenesmus according to the size and site of tumour [7].
On CT scan, the tumours appear well defined, round, mural masses with homogeneous pattern of tumour attenuation, both with and without IV contrast enhancement [8]. The main differential diagnosis here is GIST as it is the most common submucosal tumour of the gastrointestinal tract. GISTs, however, have a much more heterogeneous appearance on CT as compared to schwannomas because of the presence of haemorrhage, necrosis, and cystic change. The caveat here is the minority of non-malignant and small GISTs, whose CT findings overlap with those of schwannomas [8].
Mucosal biopsies are often inconclusive as the tumour lies in submucosa. Deep submucosal biopsies or submucosal resections can differenciate it from other submucosal GI Tumours like GISTs, neuro-endocrine tumours and leiomyomas [2, 9]. Definitive diagnosis is by immunohistochemistry as they stain strongly positive for S100. It is essential however to confirm the diagnosis of schwannoma as the other differentials like GISTs have much higher malignant potential and can recur.
In an overwhelming majority of cases (98%), they are reported to be benign with a very low mitotic index, although few cases of loco-regional metastases have been reported [2].
The best management option is surgical resection, with negative resection margins, without the need for radical resection [10]. Endoscopic resection can be attempted in cases where the diagnosis is confirmed prior to surgery [8].
Conflict of Interest statement
None declared.



