-
PDF
- Split View
-
Views
-
Cite
Cite
Débora Melo, Joana Marantes Pimenta, Valter Paixão, José Cortés, Emilia Duro, Fátima Caratão, Metastasis of renal cell carcinoma to the parathyroid gland 12 years after radical nephrectomy, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjz032, https://doi.org/10.1093/jscr/rjz032
Close - Share Icon Share
Abstract
Renal cell carcinoma (RCC) accounts for 2–3% of all malignant tumors in adults. RCC is well-known for its propensity to metastasize to unusual sites, and late metastasis, even after several years, is common. Involvement of the parathyroid gland has only four reported cases in literature. A 62-year-old Caucasian man was referred to our department due to an enlarging cervical mass. The patient’s relevant past medical history included a left nephrectomy for RCC 12 years ago. After right thyroid lobectomy and isthmectomy, histopathology revealed an intrathyroidal nodule corresponding to the parathyroid gland with metastatic RCC. Approximately one-third of RCC subjects with apparently localized disease will develop metastasis, even several years after nephrectomy. The literature is sparse regarding the most appropriate follow-up approach for these patients. We describe a rare case of nodular goiter of the thyroid gland concurrent with metastatic RCC to an intrathyroidal parathyroid gland, without disseminated systemic metastasis.
INTRODUCTION
Renal cell carcinoma (RCC) is a lethal tumor that accounts for ~3% of all adult malignancies [1]. The introduction and widespread use of sophisticated imaging modalities has resulted in a significant increase in the incidental detection of kidney tumors. Nowadays more than 70% of all renal cancer cases are detected as incidental findings on imaging studies obtained for unrelated reasons [1, 2].
RCC is characterized by unusual metastatic sites and paraneoplastic syndromes. The development of metastatic disease is a sequential process where cancer cells depart from the primary tumor via the blood supply or lymphatic chain and deposit at proximal or distant sites. This metastatic pathway is not always predictable as in the case of renal cancer, which is notorious for its complex lymphatic drainage.
Parathyroid gland malignancies are considered rare. The most common of these tumor types is the primary parathyroid carcinoma.
Metastatic spread from other sites to the parathyroid gland occurs in up to 12% of autopsy specimens [3]. Women are affected more commonly than men (5.8:1), with a mean age at presentation of 58.5 years. The most common primary sites of malignancies that metastasize to the parathyroid glands are breast carcinomas (66.9%), melanoma (11.8%) and lung carcinoma (5.5%). Metastasis is nearly always identified as part of widely metastatic disease, with only five reported cases as isolated metastasis [4].
Here we describe the second case in literature of an intrathyroidal parathyroid gland containing renal clear cell metastasis, with the goal of informing and providing a reference for better clinical judgment in cases of metastasis to the head and neck presented several years after initial diagnosis.
CASE REPORT
A 62-year-old Caucasian man was referred to the Department of Surgery of our Hospital in October 2017 due to an enlarging mass in the right cervical region with two months evolution. The primary associated symptom was dyspnea in the supine position.
Past medical history included depression and bladder carcinoma treated with RTU-V and chemotherapy in 2010. The patient had also been treated for a T1N0M0 RCC with left nephrectomy 12 years prior and had been disease free since then. Drug history included paroxetin, mexazolam and clomipramine.
At physical examination we found a 4 cm right thyroid nodule, mobile, without palpable lymph nodes.
The ultrasound scan revealed an asymmetrical enlargement of the thyroid gland, containing a solid nodule with regular borders and peripheral vascularity in the right lobe measuring 49.3 × 30.2 mm2. The left lobe did not have any relevant findings.
Subsequently the patient underwent fine-needle aspiration (FNA) cytology analysis which resulted in the classification of the thyroid nodule as Thy2. Additionally, thyroid function tests were normal.
The patient underwent an uneventful right thyroid lobectomy and isthmectomy, in May 2018. The postoperative period was unremarkable with discharge at the second postoperative day.
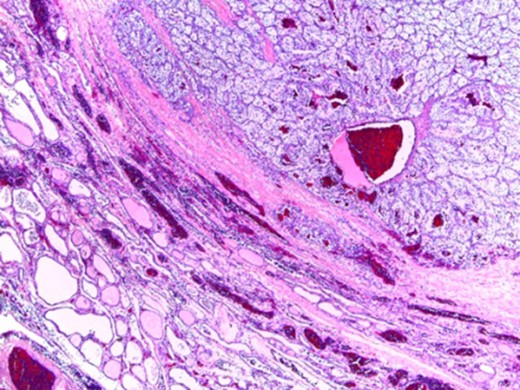
Gross examination revealed a thyroid lobe and isthmus weighing 52 g. The right lobe measured 3.8 × 5.8 × 3.5 cm3 while the isthmus measured 2.5 × 1.5 × 1 cm3. The specimen was transected revealing an intrathyroidal nodule, apparently encapsulated, yellow in color, with cystic and hemorrhagic areas measuring 4.2 × 3.5 cm2 as presented in Fig. 1.

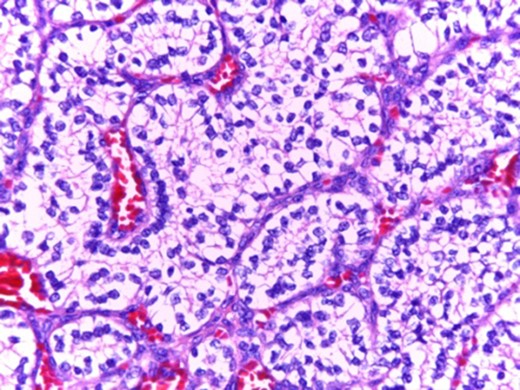
In microscopic evaluation the tumor had a predominantly ‘clear cell’ morphology, typical of RCC as shown in Figs 2 and 3.
Normal thyroid tissue on the lower left corner; clear cells in the upper right quadrant.
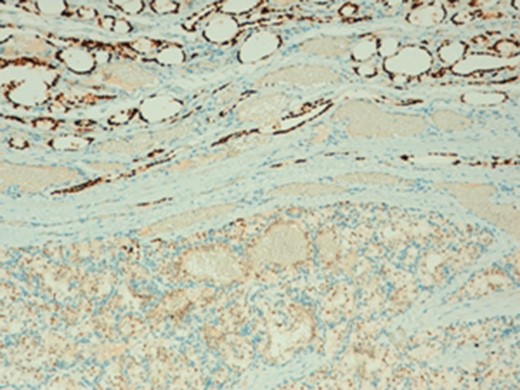
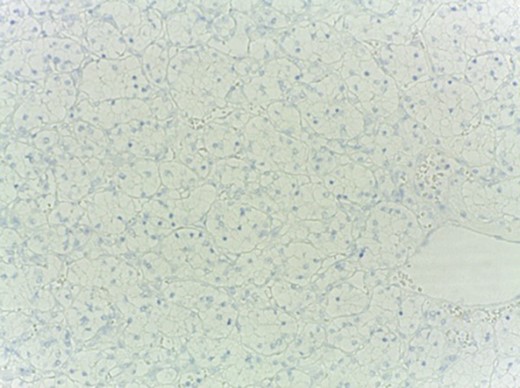
The histologic diagnosis was aided by the use of immunohistochemistry which was positive for PAX8 (Fig. 4) and CD10, and negative for thyroid transcription factor 1 (TTF-1) (Fig. 5), vimentin and chromogranin.
Additionally, the postoperative levels of PTH and calcium were within normal limits.
Currently, the patient remains alive nearly 6 months after the procedure without clinical evidence of disease.
DISCUSSION
RCC patients and metastatic RCC (mRCC) patients represent an underserved pool in the realm of cancer treatment. As the world’s population ages and the prevalence of risk factors (obesity, hypertension) increases, the burden of mRCC is foreseen to increase significantly [5].
RCC metastasis to the head and neck, although uncommon, must be considered when evaluating lesions in this region. This is especially true for those patients with a positive history of RCC, even if they have experienced extensive symptom-free periods.
Thus, the single case reports of isolated metastatic disease to the parathyroid glands alone, as the only metastatic finding in living patients are exceptional. It is of note that metastatic RCC (clear cell carcinoma specifically) to parathyroid glands is very infrequently reported.
Metastatic RCC most commonly retains the typical ‘clear cell’ histology of the primary tumor, which is an important clue to its recognition [6].
Bauer et al. [4] reviewed metastases to the parathyroid glands from 1950 to 2017 and found 127 cases, with four case being from RCC which included only one intrathyroidal parathyroid metastasis. Metastatic disease from other cancers to a benign parathyroid gland or to a parathyroid adenoma probably suggests a grave prognosis given that it can indicate widespread of metastatic disease; however, isolated metastasis to the parathyroid may occur [7].
Importantly, the differential diagnostic consideration of a metastatic clear cell carcinoma within the clear cell parathyroid gland parenchyma may prove challenging since both tumors could be PAX8 and RCC immunoreactive [8,9]. However, a positive reaction with CAIX and CD10 and a negative reaction with chromogranin and parathyroid hormone studies can help confirm a RCC origin [4,9].
The goal of this study is to provide pathologists, endocrinologists and surgeons with additional knowledge surrounding this rare entity and to increase diagnostic awareness. The contribution of case reporting should not be underestimated since many of our classical clinical teachings have originated from the observation of isolated case reports [1,9].
Conflict of Interest statement
None declared.



