-
PDF
- Split View
-
Views
-
Cite
Cite
Suy sen Hung Fong, Sahned Jaafar, Subhasis Misra, Vijay Narasimha, Scrotal hematoma with pseudo-aneurysm after transfemoral catheterization, Journal of Surgical Case Reports, Volume 2019, Issue 2, February 2019, rjy310, https://doi.org/10.1093/jscr/rjy310
Close - Share Icon Share
Abstract
Transfemoral catheterization continues to be a safe and popular approach for the evaluation of cardiac and limb ischemia. In spite of the use of vascular closing devices, complications can still arise, and rarely, scrotal hematoma with groin swelling in males, which could cause significant morbidity and possibly mortality in those patients at risk. Understanding the different presentations and different ways of management of scrotal hematoma could potentially prevent significant urological complications and exsanguination. This is a case report of a patient who suffered this rare complication that can be used as a comparison with the other few reported cases.
INTRODUCTION
Transfemoral catheterization is a relative safe, minimally invasive procedure to assess coronary arteries and limb ischemia and subsequently revascularization with the placement of a stent or balloon angioplasty. However, complications can still manifest as bleeding, infection, hematoma, pseudo-aneurysm, arteriovenous (AV) fistula formation and femoral artery thrombosis [1]. In spite of appropriate use of vascular closing devices (VCD) and its lower rate of vascular complications as compared to manual compression [2, 3], there have also been reported rare cases of scrotal hematoma following post-transfemoral catheterization for coronary intervention [4–7]. We report a similar case of scrotal and right groin hematoma post-transfemoral vascular access, but for evaluation of limb ischemia.
CASE PRESENTATION
A 72-year-old male with history of penile implant, hypertension, hyperlipidemia, severe peripheral vascular disease with extensive smoking history presented in clinic for severe bilateral lower extremities claudication. Doppler exam showed weak monophasic flow bilaterally. Patient also had a history of left popliteal stent placement and has been taking aspirin and Plavix since then. CT angiography of the lower extremities showed critical stenosis of superficial femoral artery of both lower extremities and a patent stent on the left popliteal artery. Decision was made to perform bilateral lower extremities angiograms via a transfemoral approach with possible revascularization of the right lower extremity (LE) first and then the left side on two different procedures one week apart. Both procedures were accessed through a transfemoral approach that involved balloon angioplasty of the left (L) and right (R) superficial femoral artery (SFA) and left proximal popliteal artery. No immediate post procedure complications were noted, VCDs were deployed and hemostasis was achieved on both occasions. Patient was discharged same day and aspirin and Plavix were resumed.
On the following day after the right transfemoral access approach, patient presents to ED with R groin and scrotal pain. On evaluation, severe tenderness on the R groin and scrotum was noted associated with worsening swelling and ecchymosis (Fig. 1). Vitals were within normal limits and initial hemoglobin of 12 g/dl. Ultrasound of the right groin showed a 6.3 × 4.0 × 4.9 cm hematoma (Fig. 2), his duplex ultrasound of bilateral testicle showed diminished blood flow on the right compared to the left (Fig. 3). CT of the pelvis revealed a pseudo-aneurysm on the R groin originating from the common femoral artery (CFA) measuring 2.5 × 1.4 cm and extending into the R inguinal canal, filled with hemorrhage and extension into the R scrotum that measures 13.7 × 6.4 × 6.6 cm (Fig. 4). During his clinical course, he has been hemodynamically stable in spite of drops in daily hemoglobin from 12, 8.9, 6.9, 5.9 g/dl, respectively, requiring two units of blood transfusions on hospital Day 3, and achieving a rise in hemoglobin to 8.6 g/dl. Patient then underwent an ultrasound-guided thrombin injection of the pseudo-aneurysm by the interventional radiologist without any complications and without any evidence of recurrence on ultrasound on the following day. Urology was consulted and offered no urologic interventions as his symptoms were improving. The scrotal and groin hematoma subsequently decreased in size. Patient was discharged on hospital Day 6 with aspirin and Plavix. Patient was followed up in clinic with no complains. On exam, there was a decreasing scrotal and R groin swelling/ecchymosis and improvement of penile swelling.

Initial ED appearance of scrotal hematoma and right groin swelling.

Ultrasound of the right groin showing 6.3 × 4.0 × 4.9 cm hematoma.
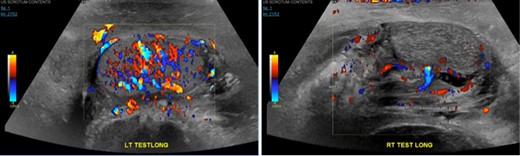
Right testicle is heterogeneous in texture and demonstrates relatively attenuated vascular flow compared to the left.
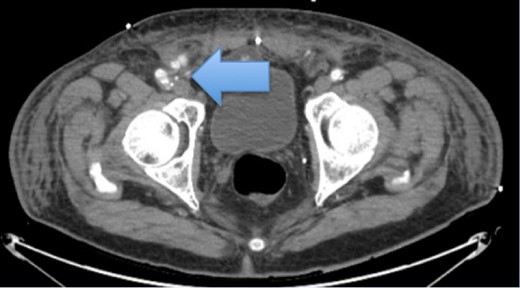
Pseudo-aneurysm from right CFA that extends obliquely measuring up to 2.5 × 1.4 cm. The pseudo-aneurysm appears to extend into the right inguinal canal, filled with hemorrhage extending into the inferior aspect of the right scrotum as well.
DISCUSSION
Transfemoral approach continues to be the standard technique for vascular access due to its optimal catheter control and immediate access to large diameter devices as compared to trans-radial approach in coronary interventions [8]. In spite the use of VCD, which reduces the vascular complication rate as compared to manual compression and providing earlier ambulation post catheterization [2, 3], associated complications can still arise following vascular access including bleeding, hematoma, infection, pseudo-aneurysm, AV malformation [1]; however, due to the increase popularity of the transfemoral approach involving the groin, it is anticipated to have an increase in urologic complication involving groin hematoma and scrotal edema [4]. Bleeding above the inguinal ligament such as retroperitoneal hemorrhage and bleeding from the inferior epigastric vessel through the pre-peritoneal space both have the potential to dissect down into the spermatic cord and into the inguinal canal, causing groin and scrotal hematoma [4, 9].
Few other case reports have been published with similar complications and symptoms of groin and scrotal pain along with drastic drop of hemoglobin [4–7]. On these four case reports, the clinical presentations and managements associated with scrotal hematoma had some similarities and differences (Table 1). The most common manifestation was inguino-scrotal swelling and pain associated with ecchymosis. All fours cases reported were from patients who underwent cardiac catheterization and only two cases reported used of anticoagulants due to a history of drug eluting stent placement [5, 7]. Despite that majority of the reported cases used VCD, groin and scrotal hematoma was inevitable, most commonly from a CFA injury with some cases presenting with sign and symptoms of hemorrhagic shock with a drop of hemoglobin of approximately 2 g/dl. Scrotal hematoma can lead to signs and symptoms of hemorrhagic shock [4, 5, 7], whereas some may be hemodynamically stable regardless of the significant low level of hemoglobin [6]. Interestingly, one of the reported cases with hemorrhagic shock was successfully managed conservatively with blood transfusions [5].
| Case reports . | Polavarapu et al. . | Kumar et al. . | Thomas et al. . | Askari et al. . |
|---|---|---|---|---|
| Presentation with hemorrhagic shock | Not present | Present | Present | Present |
| Anticoagulation | N/A | Tigagrelor and aspirin | N/A | Plavix and aspirin |
| Use of vascular closing device | Used | Used | Not used | Used |
| Mechanical compression | Not used | Not used | D-stat hemostatic bandage with manual compression | Not used |
| Injured vessel | Right common femoral artery (CFA) | R CFA | Right inferior epigastric artery | R CFA |
| Drop in hemoglobin (g/dl) or hematocrit (%) | 5.7 g/dl | 11.3 g/dl and 33.4% | 21% | 7.5 g/dl and 23.3% |
| Interventions or conservative management | Groin exploration and repair of CFA | Conservative management | Groin exploration with vessel ligation | Right femoral angiography with left femoral approach |
| Case reports . | Polavarapu et al. . | Kumar et al. . | Thomas et al. . | Askari et al. . |
|---|---|---|---|---|
| Presentation with hemorrhagic shock | Not present | Present | Present | Present |
| Anticoagulation | N/A | Tigagrelor and aspirin | N/A | Plavix and aspirin |
| Use of vascular closing device | Used | Used | Not used | Used |
| Mechanical compression | Not used | Not used | D-stat hemostatic bandage with manual compression | Not used |
| Injured vessel | Right common femoral artery (CFA) | R CFA | Right inferior epigastric artery | R CFA |
| Drop in hemoglobin (g/dl) or hematocrit (%) | 5.7 g/dl | 11.3 g/dl and 33.4% | 21% | 7.5 g/dl and 23.3% |
| Interventions or conservative management | Groin exploration and repair of CFA | Conservative management | Groin exploration with vessel ligation | Right femoral angiography with left femoral approach |
| Case reports . | Polavarapu et al. . | Kumar et al. . | Thomas et al. . | Askari et al. . |
|---|---|---|---|---|
| Presentation with hemorrhagic shock | Not present | Present | Present | Present |
| Anticoagulation | N/A | Tigagrelor and aspirin | N/A | Plavix and aspirin |
| Use of vascular closing device | Used | Used | Not used | Used |
| Mechanical compression | Not used | Not used | D-stat hemostatic bandage with manual compression | Not used |
| Injured vessel | Right common femoral artery (CFA) | R CFA | Right inferior epigastric artery | R CFA |
| Drop in hemoglobin (g/dl) or hematocrit (%) | 5.7 g/dl | 11.3 g/dl and 33.4% | 21% | 7.5 g/dl and 23.3% |
| Interventions or conservative management | Groin exploration and repair of CFA | Conservative management | Groin exploration with vessel ligation | Right femoral angiography with left femoral approach |
| Case reports . | Polavarapu et al. . | Kumar et al. . | Thomas et al. . | Askari et al. . |
|---|---|---|---|---|
| Presentation with hemorrhagic shock | Not present | Present | Present | Present |
| Anticoagulation | N/A | Tigagrelor and aspirin | N/A | Plavix and aspirin |
| Use of vascular closing device | Used | Used | Not used | Used |
| Mechanical compression | Not used | Not used | D-stat hemostatic bandage with manual compression | Not used |
| Injured vessel | Right common femoral artery (CFA) | R CFA | Right inferior epigastric artery | R CFA |
| Drop in hemoglobin (g/dl) or hematocrit (%) | 5.7 g/dl | 11.3 g/dl and 33.4% | 21% | 7.5 g/dl and 23.3% |
| Interventions or conservative management | Groin exploration and repair of CFA | Conservative management | Groin exploration with vessel ligation | Right femoral angiography with left femoral approach |
The level of hemodynamic instability will depend on the degree and acuity of the hemoglobin drop and whether there is evidence of any active bleeding. The differences in clinical and surgical management would depend on the surgeon’s judgment based on the patient’s clinical presentation; their response to blood transfusions and whether any further drop in hemoglobin is seen. Given that scrotal hematoma is a urological complication, an urology consult is warranted for the possibility of scrotal exploration and salvage of testicles from ischemia [4]. In summary, there has not been any mortality cases associated with this rare complication after a transfemoral vascular access, but predicting those who may be at risk would definitely help prevent significant morbidity and mortality in these patients.
CONFLICT OF INTEREST STATEMENT
None declared.



