-
PDF
- Split View
-
Views
-
Cite
Cite
Lina H Raffa, Rhino–orbito–cerebral mucormycosis following penetrating keratoplasty, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz314, https://doi.org/10.1093/jscr/rjz314
Close - Share Icon Share
Abstract
Rhino–orbito–cerebral mucormycosis (ROCM) is a potentially devastating fungal infection with a significant fatality rate. Early diagnosis and prompt management are crucial to ensure a favorable outcome due to the recognized rapid progression. This case is a rare presentation of ROCM in a patient with uncontrolled diabetes following a corneal transplant. The procedure required early surgical resection in the first 30 hours of hospitalization. The patient received wide-spectrum antibiotics and antifungal treatment and underwent extensive debridement of the necrotic area. A high index of suspicion is needed to diagnose ROCM. Any diabetic patient with sinonasal disease and/or cranial nerve involvement, irrespective of their serum glucose or glycated hemoglobin levels, is a candidate for prompt evaluation to exclude mucormycosis. The rapid evolution of our case highlights the importance of treating ROCM promptly and aggressively.
INTRODUCTION
Mucormycosis is a severe, life-threatening fungal infection characterized by rapid progression in immunocompromised patients [1]. Rhino–cerebral, pulmonary and cutaneous sites are more frequently involved [1]. Diabetic patients typically develop the rhino–cerebral form [2], which constitutes about 30–50% of all mucormycosis cases [3]. Mortality from dissemination to the brain has been reported to reach up to 100% [4]. Any medical management trial of true mucormycosis may result in delayed treatment with fatal consequences because tissue necrosis due to the disease results in poor penetration of the antifungal therapy to the infection site [1]. Clinical vigilance and prompt aggressive surgical and antimicrobial management are necessary to limit the well-known sequelae of mucormycosis, including vision loss and death [5].
A literature review using MeSH words ‘mucormycosis’ and ‘penetrating keratoplasty’ revealed no similar reported cases.
CASE REPORT
An 87-year-old male presented to the emergency department with generalized weakness as a case of diabetic ketoacidosis. He had a history of uncontrolled diabetes mellitus with chronic renal failure and left below knee amputation. He had undergone a penetrating keratoplasty procedure in the right eye in India 10 days prior to admission.
On examination, the patient was found to be afebrile, confused, generally weak and incoherent. Complete ophthalmoplegia despite no marked signs of inflammation with non-reactive pupils and no view of the posterior fundus were marked (Fig. 1). A reduction in right visual acuity from ‘counting fingers’ to ‘light perception’ was noted. An ophthalmic B scan revealed infiltration of the right globe. A computed tomography (CT) scan of the orbit and brain revealed signs of cavernous sinus thrombosis versus orbital cellulitis (Fig. 2A and B).

Image taken on initial presentation. Note the violaceous discoloration along the right zygomatic area with mild soft tissue swelling in that area; however, there was no obvious orbital involvement.
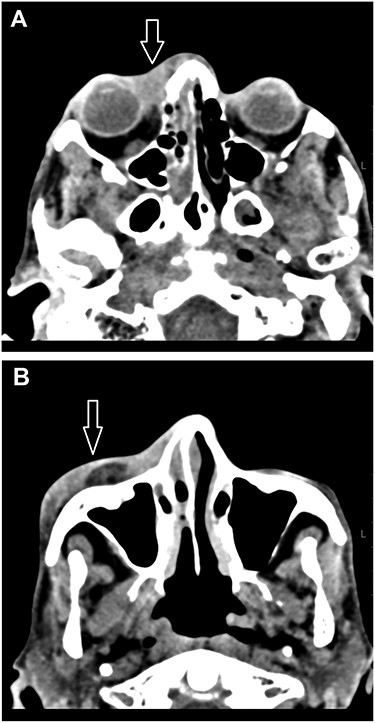
(A, B) A CT scan of the orbit and brain revealed soft tissue swelling in the pre-septal area (white arrow) and partial opacification of the right nasal cavity (A). The swelling extended to the lateral aspect of the anterior portion of the right zygomatic arch (white arrow; B).
The patient was promptly started on intravenous meropenem, vancomycin and heparin. The next day, the patient’s level of consciousness deteriorated; he developed seizures and orbital involvement of the infection worsened. A CT brain venography revealed poor enhancement of the right cavernous sinus (Fig. 3). A lumbar puncture sample was later found to be negative for microorganisms. The patient was evaluated by an ear–nose–throat (ENT) specialist who made a provisional diagnosis of mucormycosis due to the presence of micronasal abscesses and right alar blackish discoloration. Intravenous amphotericin B and caspofungin were added to his treatment.
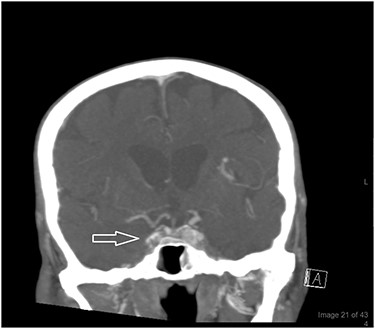
A CT brain venography revealed poor enhancement of the right cavernous sinus (white arrow) the following day. His sinuses were initially clear but later showed partial opacification of the maxillary and sphenoid sinuses with fluid levels denoting acute insult. Increased right pre-septal thickening and abnormal infiltration of the right eye were noted as well.
A rapid progression to the orbit and a gangrenous area on the tip of the nose was observed (Fig. 4). The suspicion of mucormycosis was confirmed, and the option of surgical debridement was discussed with the patient’s family. Written informed consent was obtained from the next of kin to proceed with the surgery.

Image taken on the second day of admission. Note the spontaneous laceration (not noted on admission) extending from the edge of the right medial canthus to the bridge of the nose with no signs of bleeding and the worsening of the blackish discoloration of the midface and nose bridge.
The ophthalmology, ENT and maxillofacial teams performed a right orbital exenteration along with a widespread deep excision of the necrotic area (Fig. 5). Peri-operative intravenous antibiotics and antifungals were administered as per hospital protocol for severe skin sepsis, and the patient was transferred to the intensive care unit for post-operative support. The patient had a Glasgow Coma Score of three post-operatively.

Intraoperative view of the debridement of necrotic tissue in the affected area in the right eyelids, right cheek and bridge of the nose. The paranasal sinuses were debrided endoscopically as well.
On examination the next day, the patient remained clinically septic with a clear extension of necrotic tissue beyond the existing surgical margins. The right ear and left eye were involved. After discussion with the family, they refused further surgical intervention. Blood cultures were negative; however, a microscopic examination of the patient’s tissue samples revealed invasive broad fungal hyphae yeast cells with acute and chronic inflammatory cells, necrotic tissue and suppurative microabscesses consistent with mucormycosis. These findings confirmed the clinical suspicion.
Extensive tissue debridement and antifungal therapy were not successful in controlling the rapid fungal invasion of the tissues, and the patient subsequently died 4 days after admission.
DISCUSSION
Mucormycosis is an uncommon infection characterized by rapidly progressive vascular invasion and tissue necrosis. When the orbital tissues are involved, the infection can rapidly cause permanent loss of vision and a potentially fatal extension to the brain [5].
This report shows why it is important to consider rarer causes of soft tissue infections in cases with presumed cellulitis. The diagnosis of mucormycosis is mostly made based on a high index of clinical suspicion. While antibiotic treatment alone can suffice in successfully managing most cellulitis cases, aggressive management is required in patients with mucormycosis [5]. In mucormycosis, there is an invasion of the blood vessels and a violaceous discoloration of the skin; however, these clinical features typically appear as the disease progresses. Thus, mucormycosis and orbital cellulitis are not usually easily distinguishable at disease onset [6].
Advanced age (>50 years) was indicated as a risk factor for death. Other risk factors, such as steroid use and diabetes mellitus, are known to predispose patients to mucormycosis [7]. One of the rising nosocomial infections observed in organ or hematopoietic transplanted patients is mucormycosis, possibly due to the associated iron overload or steroid use [1]. However, to our knowledge, this is the first report of rhino–orbito–cerebral mucormycosis following a corneal transplant. Reported incidences of fungal infections post-keratoplasty remain low (4 of 17 035 donor corneas) and have been attributed to donor–host–transmission regardless of whether they were eye bank-prepared or not [8].
Mortality from mucormycosis was reported to range from 30 to 100% [4, 9] and is attributable to several factors, including the spread of the infection to the brain. Antimicrobials may not reach the infected site due to thrombosis of the blood vessels. Therefore, antimicrobial therapy must be combined with prompt surgical debridement of the affected tissue beyond an area of obvious clinical infection. Surgical debridement decreases the microbial load and helps to decrease the mortality. While a delay in diagnosis is often responsible for the mortality associated with the disease, the diagnosis at our institute was made relatively quickly. Nevertheless, our patient was an extremely high-risk case.
CONCLUSION
Rhino–orbito–cerebral mucormycosis is a severe, emergent and fatal infection requiring the intervention of a multidisciplinary team, including internists and surgical and infectious disease specialists. Ophthalmologists should have a high index of suspicion in immune-deficient patients presenting with exophthalmia, progressive periorbital or facial edema, or necrosis, with or without cranial nerve involvement. Early diagnosis and urgent surgical debridement are crucial to eradicate the infection successfully and improve patient outcome.
ACKNOWLEDGEMENTS
This report has been reviewed and approved by the Research Ethics Committee at the Faculty of Medicine, King Abdulaziz University Hospital. I would like to thank the treating teams for their cooperation in patient management.
Conflict of interest statement
The author declares that there is no conflict of interest regarding the publication of this article.
FUNDING
The author received no financial support for the research, authorship, and/or publication of this article.
Consent
Informed consent was obtained from the next of kin to publish this report for research purposes.



