-
PDF
- Split View
-
Views
-
Cite
Cite
Christopher L Kalmar, Curtis E Bower, Laparoscopic repair of interparietal abdominal wall hernias, Journal of Surgical Case Reports, Volume 2019, Issue 11, November 2019, rjz319, https://doi.org/10.1093/jscr/rjz319
Close - Share Icon Share
Abstract
Interparietal hernias are rare abdominal defects where intraabdominal contents protrude between layers of the abdominal wall. There is limited experience using laparoscopic technique for repairing substantially large interparietal hernias. Computed tomography scans of both cases herein demonstrated intact external oblique, but the internal oblique and transversus abdominis were widely detached from the linea semilunaris. Our experience demonstrates the largest interparietal hernias treated entirely with laparoscopic repair, which successfully resolved symptoms and abdominal wall irregularity, as well as allowed discharge on the first postoperative day without complication.
INTRODUCTION
Interparietal hernias are rare abdominal defects where intraabdominal contents protrude between layers of the abdominal wall. Interparietal hernias present a diagnostic challenge because the superficial layers of the abdominal wall remain intact and obscure the physical exam. Moreover, interparietal hernias may be difficult to diagnose on radiographic or ultrasound imaging. Consequently, many interparietal hernias are diagnosed only upon surgical exploration [1]. Herein, we present the largest interparietal hernias repaired entirely with laparoscopic technique.
CASE REPORT
Case A
An 84-year-old female presented for evaluation of left upper abdominal quadrant bulge which had been present after left flank incision for anterior placement of lumbar spine hardware 4 months prior. She noticed an abdominal asymmetry a few days after this procedure. She denied pain with protrusion but described pressure discomfort that was exacerbated by straining and relieved with rest. Protrusion was exacerbated by recumbent position and relieved with upright position.
Physical exam was significant for large left flank and left upper abdominal quadrant hernia, which was partially reducible and nontender.
Computed tomography (CT) imaging of the abdomen and pelvis did not demonstrate clear evidence for an incisional hernia in the left flank region. CT imaging did show that her external oblique was intact; however, the internal oblique and transverse abdominis on the left side were detached from the linea semilunaris, resulting in an interparietal hernia (Fig. 1A).
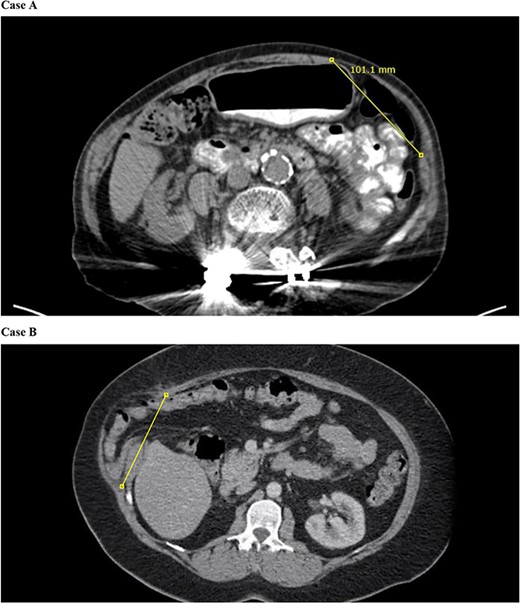
CT of the abdomen and pelvis demonstrates separation of the transversus abdominis and internal abdominal oblique from the linea semilunaris.
Initial laparoscopic survey demonstrated separation of the linea semilunaris from the internal oblique and transversus abdominis. The peritoneum on the left side was opened to allow better exposure of the muscle. Starting inferiorly just off the edge of the anterior superior iliac spine, we approximated the linea semilunaris to the internal oblique using a # 1 barbed synthetic absorbable monofilament suture (StrataFix™ PDS™; Ethicon, Somerville, NJ) running the suture in cranial direction. Thereafter, we reversed the direction of the suture to return running the suture in caudal direction prior to cutting the stitch. This noticeably decreased the bulge in her left upper quadrant (Fig. 2A). Length of this abdominal wall defect measured intraoperatively was 8–10 cm.
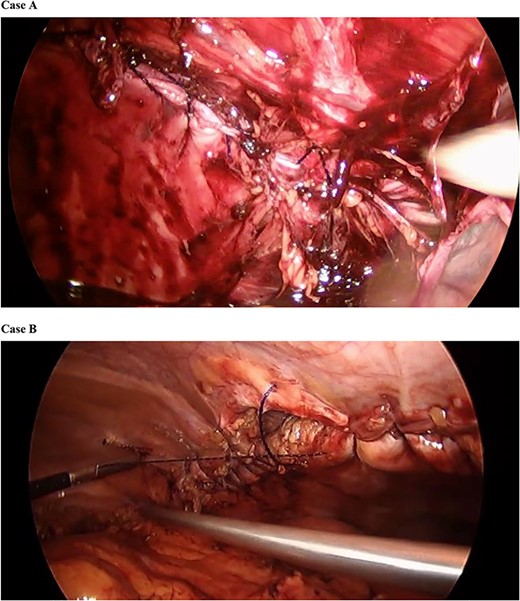
Barbed synthetic absorbable monofilament suture was used to approximate the linea semilunaris to the internal oblique.
Next, attention was directed to mesh reinforcement of the incisional hernia. We placed a 15 × 10 cm monofilament macroporous composite mesh (Symbotex™; Covidien Medtronic, Mansfield, MA) to reinforce the suture repair of her left flank incisional hernia. A centering stitch was placed allowing the mesh to be pulled up to the center of the defect repair, and thereafter, the mesh was secured to the abdominal wall with absorbable tacks (AbsorbaTack™; Covidien Medtronic, Mansfield, MA) (Fig. 3).
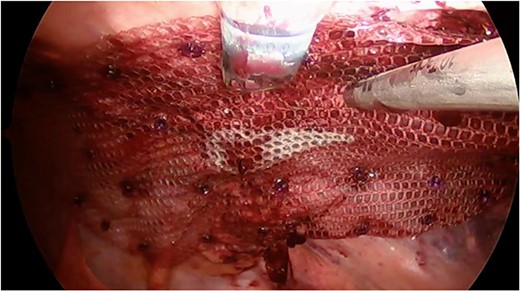
Monofilament macroporous composite mesh was placed over the abdominal wall defect with 5 cm overlap to reinforce the repair. Mesh was secured with a laparoscopic absorbable tack fixation.
Case B
A 53-year-old female presented with right flank bulge, which had been presented a few days after right flank incision for right nephrectomy for renal cancer 5 months prior. She denied chemotherapy or radiation to the area. The patient has been symptomatic with occasional burning pain exacerbated by activity.
CT imaging demonstrated a 13-cm flank hernia with the external oblique still intact; however, the internal oblique and transversus abdominis were detached from the linea semilunaris allowing herniation of non-dilated loops of bowel (Fig. 1B).
We similarly used #1 Stratafix suture, except in this case we ran sutures from both ends of the defect until they met at the middle of the hernia. We also placed transfascial sutures across the long axis of the repair to offload tension from the tissue approximation.
RESULTS
The patients did well postoperatively, and both were discharged on the morning of the first postoperative day. At 1-month and 2-month postoperative follow-up, our patients continued to do well with resolution of the abdominal wall discomfort and resolution of the abdominal wall hernias.
DISCUSSION
Incisional hernias remain a common complication after surgical procedures. Nevertheless, interparietal hernias are a rare complication. Interparietal hernias are defined as protrusions of intraabdominal contents within the layers of the abdominal wall [2]. Incidence is estimated to be ~0.1–1.6% and more often seen in adult males [3, 4]. More frequent presentation in children and adult males might indicate a possible relationship to the embryologic descent of the testes, although the de novo presentation of this pathology is not completely understood [1]. Risk factors for the development of any incisional hernia include weak abdominal wall musculature, diabetes, male sex, tobacco use and steroid use [5]. Additionally, risk factors of the surgical procedure predisposing to incisional hernias include emergency index procedure, bowel resection, poor choice of suture, poor technique and postoperative wound infection [5].
Subtypes of interparietal hernias includes superficial, interstitial and preperitoneal [6]. Superficial interparietal hernias are located between external oblique and skin or within aponeuroses of the inguinal region [6]. Interstitial interparietal hernias are located between transversalis fascia and transversus abdominis, internal oblique or external oblique [6]. Preperitoneal interstitial hernias are located between the peritoneum and transversalis fascia [6]. Among interparietal hernias, the incidence of interstitial hernias is about 60%, with the remaining two subtypes occurring at an incidence of 20% each [4].
Our experience demonstrates the largest interparietal hernias treated entirely with laparoscopic repair. The first entirely laparoscopic repair of any interparietal hernia was published last year for a 20-mm inguinal defect after robotic prostatectomy [7]. Thereafter, the literature this year notes a laparoscopic repair of a 4-cm defect after open appendectomy [8].
This case demonstrates the success of laparoscopic repair for significantly large abdominal wall defects causing interparietal hernias. Barbed suture significantly helped maintain tissue approximation of distantly opposing aspects of the muscular abdominal wall. This is important considering that any additional trocar sites for assistance to maintain suture tension between bites could add unnecessary morbidity. In addition to primary suture repair of the abdominal wall defect, we recommend mesh reinforcement. Moreover, we recommend reducing insufflation pressure during approximation of the abdominal wall defect.
In conclusion, interparietal hernias are a rare but potentially significant complication resulting after any abdominal surgical incision. Significantly large defects of this variety can be successfully managed entirely with laparoscopic technique using barbed suture for primary repair with subsequent mesh reinforcement.
Ethics Informed Consent
Institutional Review Board was not required for this case report. Informed written consent was obtained from the patient for publication of this case report and all accompanying medical history and images.
Disclosures
C.L.K. does not have any financial or nonfinancial relationships to disclose. C.E.B. receives funding from Bard Pharmaceuticals. There were no clinical decisions impacted by this participation.



