-
PDF
- Split View
-
Views
-
Cite
Cite
Shinsuke Uchida, Shun-ichi Watanabe, Yukihiro Yoshida, Aki Kobayashi, Keisuke Asakura, Kazuo Nakagawa, Aberrant mediastinal trunk of pulmonary artery, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjy359, https://doi.org/10.1093/jscr/rjy359
Close - Share Icon Share
Abstract
Anatomic variations of the pulmonary artery (PA) cause vascular injuries and result in critical mistakes. Here we report the first case of lung cancer with a fissureless left upper lobectomy, an aberrant mediastinal trunk of the lingular and basal segments of the PA. A 65-year-old man was referred to our hospital with a solid mass on the left upper lobe. A fissureless left upper lobectomy was performed due to severe incomplete lobulation. Intraoperative findings showed an extremely rare anatomic variation (left A5+A8+A9b) that arose as a common trunk from the left main PA. To prevent intraoperative injury, it is essential to consider the unexpected mediastinal inferior branch and perform a surgical procedure such as fissureless lobectomy upon encountering incomplete lobulation.
INTRODUCTION
Anomalies of the pulmonary artery (PA) are often encountered during anatomical lung resection [1]. A mediastinal inferior lobar branch of the PA is extremely rare [1–4]. In this case, the aberrant mediastinal trunk (A5+A8+A9b) arising from the left main PA ran between the superior pulmonary vein (PV) and the left upper bronchus. In this anatomical variation, the first trunk of the PA flowed into the lingular and basal segments.
CASE REPORT
A 65-year-old man with an abnormal shadow on his chest X-ray was referred to our department. Computed tomography (CT) revealed a solid mass with a 39-mm maximum diameter in the left upper lobe (Fig. 1A). He was diagnosed with lung adenocarcinoma (c-T2a N0 M0, c-stage IB according to the seventh edition of the Lung Cancer Classification). Abnormal mediastinal inferior lobar branch of the PA was not detected preoperatively. Retrospectively, a thin-section CT scan revealed that the mediastinal anatomical variation was that the first trunk of the PA flowed into the lingular and basal segments (Fig. 1B).
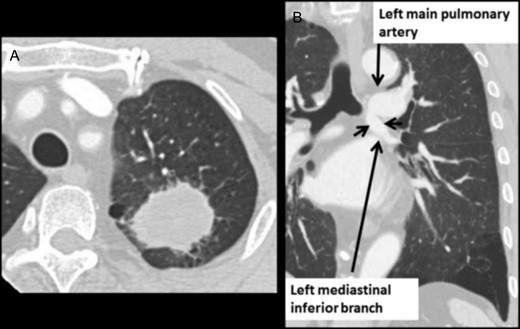
(A) Chest CT shows lung mass in the left upper lobe. (B) Chest contrast-enhanced CT shows the mediastinal anomalous inferior lobar branch.
Operative technique
The video-assisted operation was performed with a small antero-axial thoracotomy (6-cm incision). We performed a fissureless left upper lobectomy due to severe incomplete lobulation. First, we identified the superior PV. Exfoliation of the tissues behind it revealed the mediastinal inferior branch of the PA. The branch descended between the superior PV and the upper bronchus as the first branch of the PA. After we divided the superior PV by autosuturing, we exfoliated the sheaths from the PA. We identified that the A5+A8+A9b arose directly from the mediastinal branch into the lingular and basal segments. A5 was divided by autosuturing and A8+A9b was preserved. A3+A4b (mediastinal type) and A1+2a+b were identified and dissected by autosuturing. A1+2c was sealed and dissected by an energy device. The upper bronchus, which arose from the main bronchus, was detected behind the anomalous branch. The upper bronchus was dissected by autosuturing using an endostapler. The bronchial stump of the resected side was ligated with an ENDOLOOP® Ligature (Ethicon, Somerville, NJ, USA) and then elevated. Next, A4a was dissected by autosuturing. Finally, we incised between the upper and lower lobes using autosuturing and removed the left upper lobe. The operative time was 155 min with a blood loss of 26 mL. The intraoperative view (Fig. 2) and illustrated schema (Fig. 3) show the anomalous branch as A5+A8+A9b. No postoperative air leakage was detected. The thoracic tube was removed 2 days after the operation. The postoperative course was uneventful, and the patient was discharged from the hospital on the fourth postoperative day.
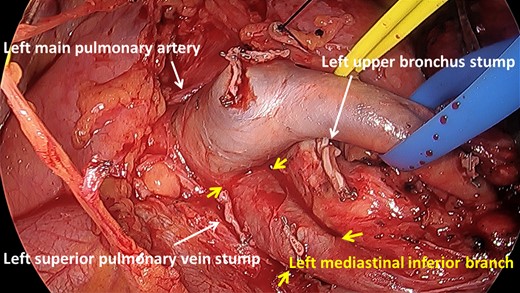
Aberrant mediastinal trunk of the pulmonary artery (A5+A8+A9b) arose from the left main pulmonary artery and ran in front of the bronchus.
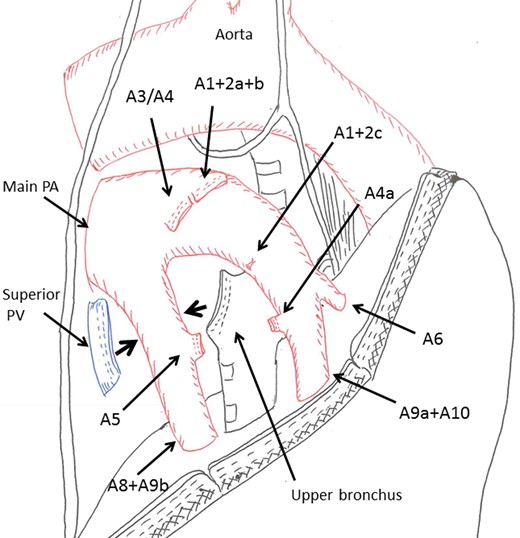
Schema illustrates the relative position of the pulmonary hilum and the mediastinal lingular and basal branches.
DISCUSSION
Anatomic variations of the PA increase the risks of vascular injury and critical mistakes. Mediastinal inferior lobar branch of the PA is extremely rare [1–4]. Previously, only 15 cases of left mediastinal inferior branch were reported [2–4]. The mediastinal anomaly of the PA was not recognized preoperatively in two of these reported cases. Among these two cases, one anomalous branch was divided intraoperatively by mistake [2].
In the present case, the mediastinal inferior branch was preserved. This rare variation ran behind the superior PV into the lingular and basal segments. This anomalous branch was not detected due to the bifurcation from the central left main PA. Although 3D-CT might be effective [5, 6], the anomalous branch was not preserved in a previous report despite its use [2]. Therefore, we must consider this rare anatomic variation.
The aim of the fissureless technique is to avoid dissection over the fissures, thereby decreasing the risk of lung parenchyma injury and postoperative air leakage [7]. We performed lobectomy using the fissureless technique in cases of emphysema and severe incomplete lobulation. This technique has been useful for exfoliation of the tissues behind the superior PV. In fact, the anomalous branch was detected behind the superior PV in the present case.
In conclusion, we hereby report the first case of fissureless lobectomy for lung cancer with an aberrant mediastinal trunk of the PA and severe incomplete lobulation. Our study results indicate that it is important to consider these mediastinal inferior branches intraoperatively.
Conflict of Interest statement
There are no conflicts of interest to declare.
REFERENCES
Author notes
Presented at the 35th Annual Meeting of the Japanese Association for Chest Surgery, Chiba, Japan, 17–18 May 2018.



