-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Lang, Preeti Chaudhri, Benign multicystic mesothelioma arising from the tunica vaginalis, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjy361, https://doi.org/10.1093/jscr/rjy361
Close - Share Icon Share
Abstract
Benign multicystic mesothelioma is an extremely rare neoplasm usually arising from the visceral mesothelium of the peritoneal cavity typically presenting in young to middle-aged women. It has been deemed an indolent tumour with a possible heritable nature, but also a possible reactive neoplasm secondary to trauma. Diagnosis relies on identifying characteristic histology of cysts separated by loose connective tissue stroma and lined by pale, flat or cuboidal mesothelial cells. A 74-year-old male presented with a painless, enlarging scrotal swelling thought to be either an epididymal cyst or hydrocele. He underwent radical orchiectomy and benign multicystic mesothelioma of the tunica vaginalis was characterized on macroscopy and microscopic examination. The potential for malignant transformation of these tumours has not been demonstrated, but they are known to recur. This infrequent presentation of a rare and poorly understood tumour with description of histologic findings may allow for improved diagnosis in other cases.
INTRODUCTION
Benign multicystic mesothelioma (BMM) is an extremely rare neoplasm usually arising from the visceral mesothelium of the peritoneal cavity which typically presents in young to middle-aged women of child bearing age. Mennemeyer and Smith first described BMM as a distinct entity in 1979 in a young lady with omental, peritoneal and pelvic involvement of a cystic structure who required multiple surgical resections for recurrence of the tumour [1]. Relatively few cases have been described in the literature and the pathogenesis of the disease has yet to be fully ascertained. Previously it has been deemed an indolent tumour with a possible heritable nature, but also as a possible reactive neoplasm secondary to trauma [2, 3]. Characteristic histologic findings of cysts separated by loose connective tissue stroma and lined by pale, flat or cuboidal cells of mesothelium have been deemed pathognomonic for BMM. Typically it has been described in mesothelium lining the abdominopelvic viscera, but infrequently involvement has been reported in the pleura [4], pericardium [5], uterus [6], spermatic cord [7] and in children [8].
We report a rare case of the disease presenting with a scrotal swelling in a gentleman who underwent radical orchiectomy and discuss the challenging nature of its diagnosis and possible histologic and immunohistochemical findings in cases of BMM.
CASE OF INTEREST
A 74-year-old male presented with a 20-year history of a slowly enlarging, painless left scrotal swelling. He had a past medical history notable for nodular malignant melanoma of the epidermis of his lower back (BRAF mutation negative) and had undergone surgical resection for a well differentiated carcinoid tumour of the terminal ileum near the time of presentation.
He underwent ultrasonography of his testes which showed a large left sided cystic area 16.6 × 8.2 × 8.8 cm3 with multiple septations and hyperechoic areas (Fig. 1). An epididymal cyst or hydrocele was initially suspected by radiology and further imaging was performed. Inflammatory change was seen in his left inguinal region on computerized tomography and he underwent left radical orchiectomy.
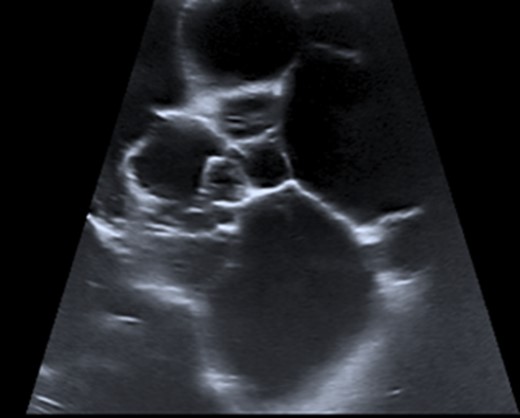
Ultrasonography of paratesticular lesion showing hyperechoic cystic regions with multiple septations.
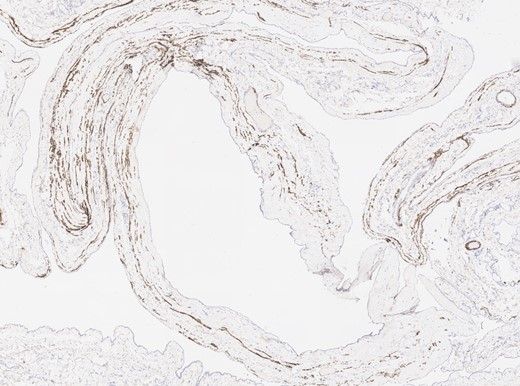
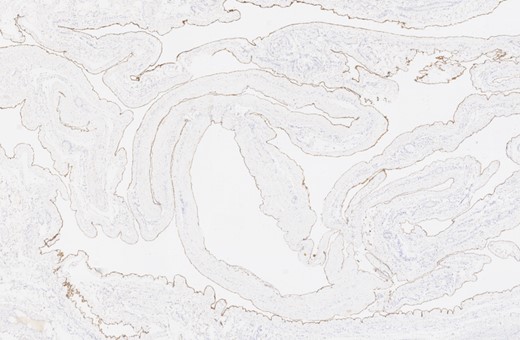
Macroscopic examination of the surgical specimen revealed an atrophic testis 40 × 30 × 30 mm3 with a large, multiloculated structure adherent to it composed of cysts of varying sizes containing serous fluid ~60 mm in maximal dimension (Fig. 2). Histological findings confirmed the presence of numerous thin-walled cysts lined by cuboidal mesothelial cells separated by delicate fibrous stroma. No atypia, mitoses or necrotic regions were observed (Fig. 3). Immunohistochemistry was undertaken and mesothelial cells were positive for WT-1 and calretinin (Figs 4 and 5) and negative for desmin in keeping with a diagnosis of BMM (Fig. 6).

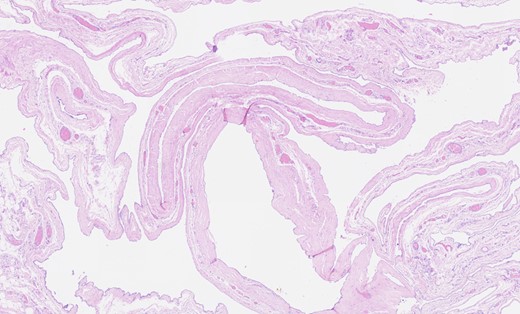
Haematoxylin and eosin staining showing thin-walled cystic areas lined by cuboidal mesothelial cells.

DISCUSSION
Confounding microscopic findings of multicystic mesothelioma with cystic lymphangiomas is possible due to similar appearances on haematoxylin and eosin staining making differentiation challenging. Accurate recognition of the mesothelial origin of cells surrounding cystic regions and appropriate selection of immunohistochemical stains will avoid misdiagnosis by surgical pathologists.
The pre-malignant potential of so-called ‘benign’ multicystic mesothelioma has been questioned with several cases described of possible malignant transformation of the tumour: one case of a lady with peritoneal lesions which had recurred with features of malignant mesothelioma following multiple surgical resections over a 10-year period and another case described of a fatal cystic hepatic neoplasm in an infant which had features of BMM as well as malignant mesothelioma [9, 10].
In conclusion, this was an unusual case of BMM of the tunica vaginalis presenting as a scrotal swelling in an elderly male which was amenable to surgical resection.
Acknowledgements
A.J. Lang was involved in literature review and preparation of the case presentation. P. Chaudhri provided expert advice, supervision and the images used in this article.
Conflict of Interest statement
Both authors declare no conflicts of interest.
Funding
No funding was obtained for this article.



