-
PDF
- Split View
-
Views
-
Cite
Cite
Burak Sezgin, Aysun Camuzcuoğlu, Hakan Camuzcuoğlu, Complete duplication of left and right external iliac vein: two case reports and review of the literature, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjy343, https://doi.org/10.1093/jscr/rjy343
Close - Share Icon Share
Abstract
The femoral vein is named as external iliac vein as it progresses in the cranial direction. In the current case report, a rare variation of the left external iliac vein that was found incidentally during pelvic lymph node dissection in a 36-year-old woman is presented. We also found the same variation at the right side in a 55-year-old woman during laparoscopic pelvic lymph node dissection. Duplication of left external iliac vein throughout its entire length was detected during the operation of the patient with diagnosis of malignant ovarian serous tumor. The other patient with duplication of the right external iliac vein was diagnosed as stage IA, grade 3 endometrial cancer. These rare variations of external iliac veins are of great importance in gynecologic oncologic surgery and other operations requiring pelvic lymph node dissection. Here, we presented and discussed the importance of this variation with the photographs taken during the operation.
INTRODUCTION
The external iliac vein is formed by the proximal continuation of the femoral vein. The inferior epigastric vein, deep circumflex iliac vein and pubic vein are the branches of the external iliac vein. The positions of external iliac veins according to their synonym arteries differ from each other. The left external iliac vein is situated completely medial to the left external iliac artery; however, on the right side its position is first medial to the left external iliac artery, then inclines posteriorly as it continues upwards.
Herein, we will present two rare cases of completely duplicated external iliac veins found incidentally during gynecologic oncologic surgery, and we will discuss the importance of these variations.
CASE REPORT 1
A 36-year-old gravida 2, para 2 female with a 2-month history of pelvic pain and menstrual dysregulation was referred to our hospital for an investigation of her symptoms. Her medical history revealed no abnormalities. In physical examination, she felt tenderness in her left lower quadrant. Transvaginal ultrasound imaging revealed a 5 cm left ovarian cystic mass. Magnetic resonance imaging of the abdomen with contrast media detected a 5 cm left ovarian cystic mass with papillary projections. Laboratory test results for cancer biomarkers were as follows; CA-125:311 U/ml (normal range <35 U/ml); CA-19-9:1100 U/ml (normal values <37 U/ml); CEA: 2.5 ng/ml (normal values <3 ng/ml); and CA-15.3:31.1 U/ml (normal values <35 U/ml). Due to suspicion of malignancy, gastroscopy and colonoscopy were performed which revealed no abnormalities. The patient’s smear and endometrial biopsy results were also negative. The patient was scheduled for an operation. We performed an exploratory laparotomy with frozen section consultation by a pathologist experienced in gynecologic oncology. We sent left salphingoopherectomy material for the frozen section. The intraoperative diagnosis was epithelial ovarian cancer. A total abdominal hysterectomy and bilateral salphingoopherectomy with pelvic-paraaortic lymph node dissection was performed. We found incidentally during the pelvic lymph node dissection that the patient’s left external iliac vein was completely duplicated (Fig. 1A). Our findings showed that the two veins lied parallel to each other throughout their length. The left external iliac artery lied lateral to the completely duplicated vein. We did not find any abnormalities on the right side.
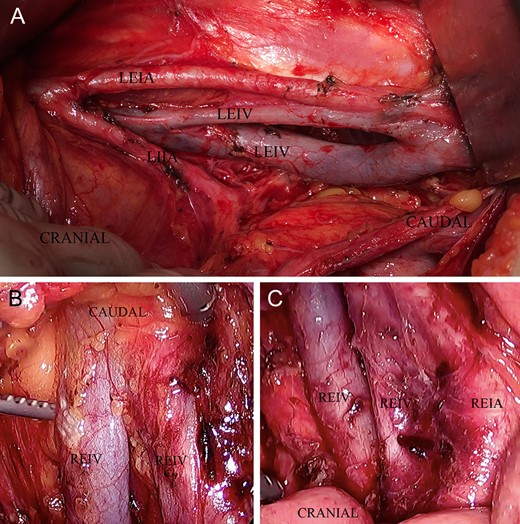
(A) shows a duplication of the left external iliac vein throughout its length, (B) shows a caudal duplication of the right external iliac vein and (C) shows a cranial duplication of the right external iliac vein.
CASE REPORT 2
A 55-year-old gravida 1, para 1 female patient who had been experiencing postmenopausal bleeding for 2 months was referred to our hospital. Endometrial pathology results revealed grade 3 endometrioid adenocarcinoma. We performed total laparoscopic hysterectomy, bilateral salphingoopherectomy and bilateral pelvic-paraaortic lymphadenectomy. During the right pelvic lymphadenectomy, we incidentally found a vein situated medially to the patient’s right external iliac vein which was a complete duplication of the right external iliac vein, from caudal to cranial. The two veins lied parallel to each other and were medial to the right external iliac artery (Fig. 1B and C). We did not find any abnormalities in the left pelvic vascular system.
DISCUSSION
In retroperitoneal operations, it is essential to know the normal anatomical structure in detail and variations of iliac veins. An unnoticed anatomic variation may cause vascular injury that can lead to a severe life-threatening hemorrhage during an operation. Deaths due to massive hemorrhages from iliac veins have been reported in literature [1].
External iliac vein variations are less common compared with other iliac vein variations. External iliac veins show diverse variations. Ajay-Chandrasekar et al. reported the unilateral aplasia of an external iliac vein, and Onkar et al. reported a case of isolated bilateral external iliac vein aplasia [2, 3]. There may also be positional variations that lie lateral to the external iliac artery. Additionally, external iliac vein may receive extra tributaries such as the obturator vein or the lumbar vein [4]. Djedovic et al. reported a case of partial duplication and an annulus formation in the left external iliac vein [5]. Hayashi et al. reported an additional right external iliac vein in their cadaver dissection, and Nishimura et al. reported a complete duplication of the left external iliac vein incidentally during a laparoscopic pelvic lymph node dissection as in our case [6, 7].
In gynecologic oncology, the vascular anatomy of the retroperitoneal space is of great importance. Unusual and complex variations in pelvic vasculature including the duplication of external iliac vein should be kept in mind especially during pelvic-paraaortic lymph node dissections. Any vascular injury in this area may cause life-threatening bleeding or complications.
ACKNOWLEDGMENTS
None.
CONFLICT OF INTEREST STATEMENT
The authors declared that they have no conflict of interests.
FUNDING
We did not have any financial support. These findings have not been presented anywhere.
AUTHOR CONTRIBUTIONS
B.S.: Project development, data analysis, manuscript writing and editing, participate in surgery. A.C.: Manuscript writing, editing and revision. H.C.: Literature research and manuscript editing, participate in surgery.
ETHICAL APPROVAL
All procedures performed in studies involving human participants were done with the ethical standards in accordance with the 1964 Helsinki declaration and its later amendments. Mugla Sitki Kocman University Ethical Committee waived the requirement for approval. Informed consent was obtained from all individual participants included in the study.



