-
PDF
- Split View
-
Views
-
Cite
Cite
Konstantinos Velaoras, Christos Plataras, Ioannis Alexandrou, George Bourikis, Maria Chorti, Efstratios Christianakis, Testicular necrosis due to complicated epididymitis and ruptured sperm granuloma in a 13-year-old boy, Journal of Surgical Case Reports, Volume 2019, Issue 1, January 2019, rjy349, https://doi.org/10.1093/jscr/rjy349
Close - Share Icon Share
Abstract
Sperm cell granuloma, also termed epididymitis nodosa, is a form of chronic epididymitis that occurs secondary to inflammation, trauma, and/or a vasectomy. We present a rare such case that to our knowledge is unique in pediatric literature: a 13-year-old boy presented with clinical and sonographic findings of epididymo-orchitis. At first, the boy was admitted for a short course of conservative treatment and was discharged. Symptoms deteriorated, he was readmitted and surgery revealed a non-twisted testis, with normal vas and vessels that ended in a necrotic testicular parenchyma. Histology showed a case of epididymitis nodosa and ruptured sperm granuloma that caused vascular compression, thrombosis and testicular necrosis. Epididymitis nodosa should be considered in cases of testicular swelling when clinical course is unusual and conservative treatment fails.
INTRODUCTION
This is a rare case that to our knowledge is unique in pediatric literature. It presented as a common case and was treated as such. During the course of treatment unusual clinical findings deemed necessary operative management which revealed rare histological findings. This case offers valuable clinical lessons, presented a diagnostic and management challenge and highlights an unusual mechanism of histopathology. Learning outcome of this article might change and improve management in similar cases.
CASE REPORT
A 13-year-old boy presented to the emergency department with a 10 hour history of painless edema and redness of the left hemiscrotum. No history of trauma, gastrointestinal symptoms, vaccination or previous episodes of epididymitis or epididymo-orchitis was referred. Physical examination showed an enlarged, soft, red but painless left hemi-scrotum. Blood tests were normal. Urine sample was sterile.
Initial sonographic findings were suggestive of epididymo-orchitis. The testis was well perfused and in normal position (Fig. 1). He was admitted for 3 days to start intravenous anti-inflammatory and antibiotic treatment and discharged under antibiotic treatment. Re-examinations were scheduled to assess treatment. On first reexamination, a week later, edema had subsided and the testis appeared hard, indurated and painless (Fig. 2). Ultrasound was still suggestive of epididymo-orchitis. Nevertheless suspicion for a testicular tumor was raised because of persistence of clinical and sonographic findings. An earlier appointment was scheduled this time. Five days later, at the second reexamination, another ultrasound showed reduced testicular perfusion that reached only the periphery of the testicular parenchyma (Fig. 3). The boy was operated as an emergency. Intraoperatively testis was non-twisted, with normal vas and vessels that ended in a necrotic testicular parenchyma. The testis was dark brown, hard on palpation and no blood came out when incised (Fig. 4). Right orchidectomy was performed. Since the exact cause of testicular necrosis was still unkown at the time of operation a left orchidopexy was performed to protect the only surviving testis from any future risk of torsion. The boy was discharged the next day. Histology showed a case of epididymitis nodosa and ruptured sperm granuloma that caused vascular compression, thrombosis and testicular necrosis (Fig. 5). More specifically, it showed proliferation of small ducts and gland-like structures in the walls of the vas deferens and epididymis in response to fluid and sperm dissection into the interstitium secondary to mechanical obstruction and increased intraluminal pressure. These findings are extremely rare in pediatric patients. The boy had an uneventful postoperative course and was discharged 2 days after surgery able to travel by sea to his home island.
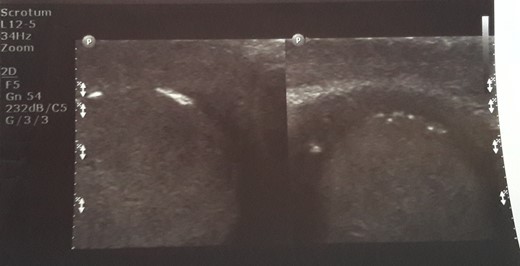
Initial sonographic findings were suggestive of orheoepididymitis.

On re-examination a week later, edema had subsided and the testis appeared hard, indurated and painless.

Five days later another ultrasound showed reduced testicular perfusion that reached only the periphery of the testicular parenchyma.

Intraoperatively testis was non-twisted, with normal vas and vessels that ended in a necrotic testicular parenchyma.
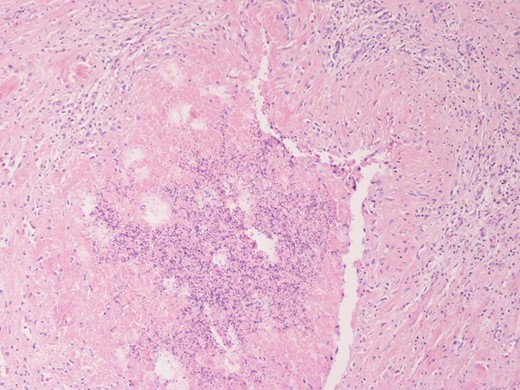
Spermatic granuloma: accumulation of sperm (center) surrounded by a granulomatous foreign body inflammatory response (upper part). H-EX 100.
DISCUSSION
Epididymitis is an inflammation of the epididymis. It is well demonstrated that most cases of epididymitis in sexually active patients are due to sexually transmitted infections. In infancy, acute epididymitis can be a systemic disease manifestation or it can be associated with an underlying genitourinary abnormality. However, its cause in prepubertal boys remains controversial. Treatment of epididymitis in children is generally based on analgesic and anti-inflammatory therapy. Most textbooks state that epididymitis is the result of an infection ascending from the bladder or urethra and should be treated with a course of antibiotics effective against usual urinary pathogens. However, there are few data to support a bacterial cause of epididymitis in children, and these treatment recommendations are not evidence-based [1–3].
Testicular infarction is an uncommon finding in pediatric age and is usually due to testicular torsion or trauma causing venous rupture with thrombosis and/or arteriolar obstruction. Other causes of segmental infarction of the testes are represented by polyarteritis nodosa, thromboangiitis obliterans and hypersensitivity angiitis [1].
Testicular loss can happen in a case of epididymitis due to vascular compression (swelling of the epididymis—inflammation of the spermatic cord) → edema → lymphatic/venous compression → arterial occlusion/thrombosis. However, this has only been described in few adult cases and has never been described in childhood [4].
Sperm cell granuloma, also termed epididymitis nodosa, is a form of chronic epididymitis seen in adults which occurs most commonly as late post-vasectomy change but also secondary to inflammation, trauma, herniorrhaphy and prostatectomy and in patients with primary infertility, chronic severe cystitis and bladder diverticula [5, 6].
Literature review revealed only one case of epididymal inflammatory pseudotumor (IPT) with incidental sperm granuloma in an adolescent and its presence in this situation was likely the result of downstream tumor obstruction [6]. So our case is unique as to the cause of testicular pathology in a child, the clinical course and outcome.
In conclusion, epididymitis is a benign condition, considered as a postinfectious disease that resolves after a few days of conservative treatment. However some cases may require surgical attention when symptoms persist despite treatment, worsen or/and are unusual. Epididymitis nodosa/sperm cell granuloma can happen in a child. In such cases, there is a possibility for ruptured granuloma and/or vascular compromise and finally testicular necrosis. Prompt surgical exploration may prevent orchidectomy.
CONFLICT OF INTEREST STATEMENT
None declared.



