-
PDF
- Split View
-
Views
-
Cite
Cite
Shin-ichi Kosugi, Hiroshi Ichikawa, Yo Sato, Eiji Sunami, Kenichiro Hirano, Takeaki Matsuzawa, Motoko Takahashi, Unusual lymph node metastasis from cancer of the thoracic esophagus, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy214, https://doi.org/10.1093/jscr/rjy214
Close - Share Icon Share
Abstract
A 76-year-old male received concurrent chemoradiotherapy, at a dose of 60 Gy with low-dose 5-fluorouracil, for cT1bN0M0 squamous cell carcinoma of the mid-thoracic esophagus. Because his primary tumor relapsed with mediastinal and right supraclavicular node metastasis 4 months after completion of chemoradiotherapy, right transthoracic esophagectomy with mediastinal and right cervical lymphadenectomy was performed. However, metastatic tumors developed deep beneath the anterior border of the trapezius muscle 2 months after esophagectomy. En bloc dissection of the adipose tissue including the tumor and the transverse cervical artery was performed, followed by adjuvant radiotherapy of 50.4 Gy to the area of dissection. The patient died of pneumonia 11 months after metastasectomy, with locally recurrent disease. We have had three cases of this unusual lymph nodes metastasis from cancer of the thoracic esophagus to date and here present the characteristic imaging findings and the possible mechanism of this unusual lymph node metastasis.
INTRODUCTION
Lymph nodes in the posterior triangle of the neck belong to the level V lymph node group in head and neck cancer, the posterior (lateral) boundary of which is the anterior border of the trapezius muscle [1]. The nodes following the transverse cervical vessels and the supraclavicular nodes are included in sublevel VB and are regarded as non-regional lymph nodes of cancer of the thoracic esophagus [1]. Supraclavicular node metastasis (SCNM) from cancer of the thoracic esophagus is occasionally seen; however, lymph node metastasis (LNM) beyond the posterior triangle is seldom seen.
CASE REPORT
A 76-year-old male underwent screening endoscopy because of a history of gastrectomy for cancer, which showed a superficial and protruding tumor in the mid-thoracic esophagus. Histological examination of the biopsy specimen confirmed well-differentiated squamous cell carcinoma. A computed tomography (CT) scan of the neck, chest and abdomen showed no evidence of metastatic disease. The tumor was clinically staged as T1bN0M0 according to the American Joint Committee on Cancer [1]. He received concurrent chemoradiotherapy at a dose of 60 Gy with low-dose 5-fluorouracil. Four months after completion of chemoradiotherapy, however, the primary tumor relapsed with mediastinal LNM and right SCNM. Right transthoracic esophagectomy with mediastinal and right cervical lymphadenectomy was performed as a salvage treatment. Two months after esophagectomy, a right neck tumor developed that was palpable at the posterior triangle, close to the anterior border of the trapezius muscle. A CT scan of the neck showed a heterogeneously enhanced tumor 25 mm in diameter located between the trapezius muscle and the levator scapulae muscle (Fig. 1). En bloc dissection of the adipose tissue including the tumor and the transverse cervical artery was performed. Histological examination revealed that 5 of the 22 retrieved lymph nodes had metastatic squamous cell carcinoma. The patient received adjuvant radiotherapy of 50.4 Gy to the area of dissection; however, died of pneumonia 11 months after metastasectomy, with locally recurrent disease that invaded right brachial plexus.
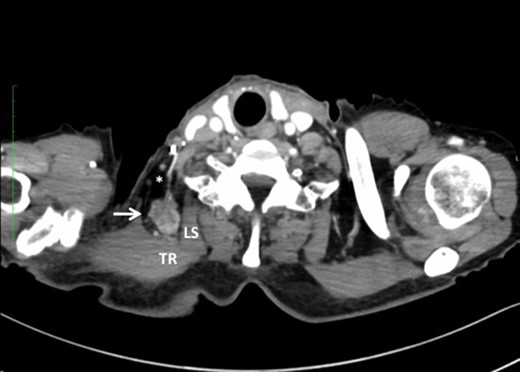
Note that the transverse cervical vessels (*) were involved in the tumor (arrow). TR, trapezius muscle; LS, levator scapulae muscle.
We have had three cases of this unusual LNM from cancer of the thoracic esophagus to date. Clinicopathological characteristics and survival are presented in Table 1. This unusual LNM developed after esophagectomy in two patients (cases 1 and 2, Fig. 2) and was found at presentation in a third patient (case 3, Fig. 3).
Clinicopathological characteristics and survival in three cases of deep transverse cervical nodes metastasis from cancer of the thoracic esophagus.
| Case . | 1 (This case) . | 2 . | 3 . |
|---|---|---|---|
| Age/gender | 77/Male | 66/Female | 48/Male |
| Tumor location | Mid-thoracic | Mid-thoracic | Mid-thoracic |
| Histology (grade) | SCC (G1) | NEC + SCC (G1) | G4* |
| Initial treatment for primary tumor | CRT + esophagectomy | Esophagectomy | No |
| Lymphadenectomy | 2-Field + right cervical | 2-Field | No |
| AJCC staging | ypT2N2M1 | pT1bN2M0 | cT4bN0M1 |
| Disease free interval | 2 Months | 4 Months | – |
| Side of SCNM | Right | Left** | No |
| Side of deep TCNM | Right | Left** | Left |
| Treatment for deep TCNM | Lymphadenectomy | No | Excision* |
| Additional treatment | Radiotherapy | No | Chemotherapy |
| Survival outcomes | Dead | Dead | Dead |
| Survival after deep TCNM development | 11 Months | 2 Months | 3 Months |
| Overall survival | 18 Months | 6 Months | 3 Months |
| Case . | 1 (This case) . | 2 . | 3 . |
|---|---|---|---|
| Age/gender | 77/Male | 66/Female | 48/Male |
| Tumor location | Mid-thoracic | Mid-thoracic | Mid-thoracic |
| Histology (grade) | SCC (G1) | NEC + SCC (G1) | G4* |
| Initial treatment for primary tumor | CRT + esophagectomy | Esophagectomy | No |
| Lymphadenectomy | 2-Field + right cervical | 2-Field | No |
| AJCC staging | ypT2N2M1 | pT1bN2M0 | cT4bN0M1 |
| Disease free interval | 2 Months | 4 Months | – |
| Side of SCNM | Right | Left** | No |
| Side of deep TCNM | Right | Left** | Left |
| Treatment for deep TCNM | Lymphadenectomy | No | Excision* |
| Additional treatment | Radiotherapy | No | Chemotherapy |
| Survival outcomes | Dead | Dead | Dead |
| Survival after deep TCNM development | 11 Months | 2 Months | 3 Months |
| Overall survival | 18 Months | 6 Months | 3 Months |
NEC, neuroendocrine carcinoma; SCC, squamous cell carcinoma; CRT, chemoradiotherapy; AJCC, American Joint Committee on Cancer; SCNM, supraclavicular nodes metastasis; TCNM, transverse cervical nodes metastasis.
*Undifferentiated carcinoma was confirmed by excisional biopsy. **Left SCNM and deep TCNM and axillary nodes metastasis developed simultaneously 4 months after esophagectomy.
Clinicopathological characteristics and survival in three cases of deep transverse cervical nodes metastasis from cancer of the thoracic esophagus.
| Case . | 1 (This case) . | 2 . | 3 . |
|---|---|---|---|
| Age/gender | 77/Male | 66/Female | 48/Male |
| Tumor location | Mid-thoracic | Mid-thoracic | Mid-thoracic |
| Histology (grade) | SCC (G1) | NEC + SCC (G1) | G4* |
| Initial treatment for primary tumor | CRT + esophagectomy | Esophagectomy | No |
| Lymphadenectomy | 2-Field + right cervical | 2-Field | No |
| AJCC staging | ypT2N2M1 | pT1bN2M0 | cT4bN0M1 |
| Disease free interval | 2 Months | 4 Months | – |
| Side of SCNM | Right | Left** | No |
| Side of deep TCNM | Right | Left** | Left |
| Treatment for deep TCNM | Lymphadenectomy | No | Excision* |
| Additional treatment | Radiotherapy | No | Chemotherapy |
| Survival outcomes | Dead | Dead | Dead |
| Survival after deep TCNM development | 11 Months | 2 Months | 3 Months |
| Overall survival | 18 Months | 6 Months | 3 Months |
| Case . | 1 (This case) . | 2 . | 3 . |
|---|---|---|---|
| Age/gender | 77/Male | 66/Female | 48/Male |
| Tumor location | Mid-thoracic | Mid-thoracic | Mid-thoracic |
| Histology (grade) | SCC (G1) | NEC + SCC (G1) | G4* |
| Initial treatment for primary tumor | CRT + esophagectomy | Esophagectomy | No |
| Lymphadenectomy | 2-Field + right cervical | 2-Field | No |
| AJCC staging | ypT2N2M1 | pT1bN2M0 | cT4bN0M1 |
| Disease free interval | 2 Months | 4 Months | – |
| Side of SCNM | Right | Left** | No |
| Side of deep TCNM | Right | Left** | Left |
| Treatment for deep TCNM | Lymphadenectomy | No | Excision* |
| Additional treatment | Radiotherapy | No | Chemotherapy |
| Survival outcomes | Dead | Dead | Dead |
| Survival after deep TCNM development | 11 Months | 2 Months | 3 Months |
| Overall survival | 18 Months | 6 Months | 3 Months |
NEC, neuroendocrine carcinoma; SCC, squamous cell carcinoma; CRT, chemoradiotherapy; AJCC, American Joint Committee on Cancer; SCNM, supraclavicular nodes metastasis; TCNM, transverse cervical nodes metastasis.
*Undifferentiated carcinoma was confirmed by excisional biopsy. **Left SCNM and deep TCNM and axillary nodes metastasis developed simultaneously 4 months after esophagectomy.
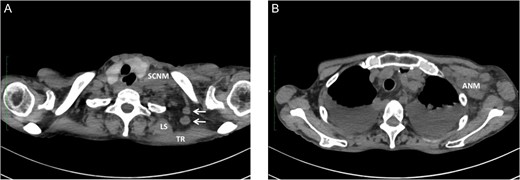
Metastasis of the supraclavicular nodes (SCNM), the nodes located between TR and LS (arrow) (A), and the axillary nodes (ANM) (B) developed 4 months after esophagectomy.
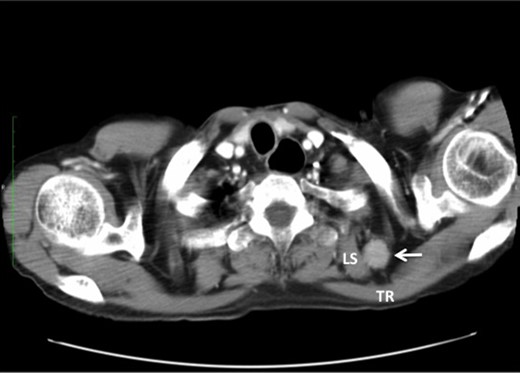
Undifferentiated carcinoma was confirmed by excisional biopsy of the tumor located between TR and LS (arrow).
DISCUSSION
The transverse cervical artery originates from the thyrocervical trunk and runs posterolaterally toward the trapezius muscle, lying transverse and anterior to the anterior and middle scalene muscles and the levator scapulae muscle, with the transverse cervical vein following a similar course [2]. Based on these anatomical considerations, the unusual LNM in our three cases might have developed along the transverse cervical vessels deep beneath the anterior border of the trapezius muscle. To our knowledge, there is no established nomenclature for these nodes, nor has metastasis to these nodes from thoracic esophageal cancer been previously reported. We therefore refer to these nodes as ‘deep transverse cervical nodes’ in this report.
One possible explanation of this phenomenon is retrograde spread from SCNM. Komatsu et al. [3] reported four cases of axillary node metastasis (ANM) of squamous cell carcinoma of the upper- and mid-thoracic esophagus. All ANM developed on the left side, with the preceding or simultaneous left SCNM. The supraclavicular nodes are well known as regional lymph nodes in breast cancer, and lymphatics from the axillary nodes are considered to communicate with the supraclavicular nodes. Based on experimental and clinical observations, they concluded that ANM might be caused by retrograde flow owing to lymphatic blockade by SCNM in esophageal cancer [3, 4]. A similar mechanism was speculated in our cases 1 and 2, in which preceding or simultaneous ipsilateral SCNM also developed. Interestingly, simultaneous ANM was also seen in case 2.
Another possible explanation is blood-borne spread rather than lymphatic spread. Toh et al. [5] reported isolated right ANM in esophageal adenocarcinoma with no prior evidence of nodal disease. They insisted that right ANM could be caused by blood-borne spread instead of lymphatic spread based on anatomical considerations; however, it is difficult to confirm whether isolated LNM as seen in case 3 is caused by skip metastasis via bypassed lymphatic flow or blood-borne spread manifested as systemic disease.
Irrespective of the metastatic pattern, deep transverse cervical nodes are non-regional lymph nodes of esophageal cancer, and patients with metastasis in these nodes are expected to have a poor prognosis. Long-term survival has been achieved in some select patients with ANM from esophageal cancer after multimodal locoregional treatment [3, 5]; however, it is still unknown whether the same strategy would be associated with a survival benefit in those with deep transverse cervical node metastasis.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- fluorouracil
- cancer
- squamous cell carcinoma
- tissue dissection
- esophagectomy
- lymph node excision
- neoplasm metastasis
- pneumonia
- radiotherapy, adjuvant
- adipose tissue
- diagnostic imaging
- esophagus
- lymph nodes
- mediastinum
- neoplasms
- lymph node dissection
- lymph node metastasis
- radiochemotherapy
- trapezius muscle
- cervical artery
- supraclavicular lymph node
- esophagectomy by abdominal and transthoracic mobilization
- metastasectomy
- thoracic esophagus



