-
PDF
- Split View
-
Views
-
Cite
Cite
Stephanie Flukes, Tonsillectomy complicated by jugular vein thrombosis and pulmonary embolism, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy202, https://doi.org/10.1093/jscr/rjy202
Close - Share Icon Share
Abstract
To report an unusual and life-threatening complication of routine tonsillectomy, and review the relevant medical literature. A Medline database search was performed to identify reports of thromboembolic complications of tonsillectomy. Thromboembolic complications following tonsillectomy are rare, and no previously reported cases of post-operative jugular vein thrombosis and pulmonary embolism are described. We report a case of an 18-year old previously healthy woman who presented with a sub-massive pulmonary embolus following tonsillectomy. It is believed that the embolus originated from a post-operative jugular vein thrombosis. This is the first report of jugular vein thrombosis and pulmonary embolism following tonsillectomy. Knowledge of this potentially life-threatening complication is vital for otolaryngologists routinely performing this procedure.
INTRODUCTION
Tonsillectomy is a common procedure. The Organization for Economic Co-operation and Development (OECD) Health Statistics surgical procedures database compiles data from 31 countries and shows tonsillectomy rates ranging between 130 and 200 per 100 000 patients [1]. Reports of thromboembolic complications are rare. When they do occur, they can be life threatening; the mortality rate of pulmonary embolism is variably reported from 8 to 13% [2]. It is therefore imperative that these complications are recognized early so that appropriate management can be implemented.
CASE REPORT
An 18-year-old female underwent tonsillectomy for recurrent tonsillitis. She was otherwise fit and well, with no past medical history and no current medications. Her father had suffered multiple spontaneous deep vein thromboses (DVT) in the past, but neither he nor the patient had been tested for coagulation disorders. The procedure was performed with sharp dissection technique, and there were no immediate complications. The patient was discharged home after overnight inpatient observation.
She re-presented to the emergency department Day 2 post-operatively with sudden onset severe dyspnoea and right-sided pleuritic chest pain. She was tachypnoeic (22 breaths per minute) and hypoxic (oxygen saturation 94% on room air). She was afebrile, haemodynamically stable, with no pain or swelling in her neck or lower limbs.
The Well’s score for pulmonary embolism was calculated to be 6 (high risk), so the patient underwent a ventilation-perfusion scan (VQ scan). This showed six areas of VQ mismatch bilaterally, consistent with multiple pulmonary emboli. Doppler ultrasound (US) showed no evidence of DVT in the lower limbs or iliac vessels. US of the neck revealed a thrombus of the left internal jugular vein (IJV), extending over a length of 4 cm. There was no clinical, biochemical or radiological evidence of infection.
The patient was commenced on an unfractionated heparin infusion. This proved difficult to manage in the post-operative period, due to recurrent minor bleeding from the tonsillectomy bed. This was managed conservatively. After 14 days, the patient was commenced on oral anticoagulation and discharged home.
DISCUSSION
To our knowledge, this is the first report of jugular vein thrombosis and pulmonary embolism following tonsillectomy [3, 4]. We identified a single case report in the literature of post-operative IJV thrombosis, without pulmonary embolism. Nix [3] reported a case of a 16 year old patient who presented 6 days post-tonsillectomy with fevers, raised white cell count, and US-confirmed IJV thrombosis. Due to the timing and associated features of the case, it is possible that the thrombosis occurred secondary to post-operative infection. This was certainly not the case in our patient, as her presentation was relatively earlier and there were no clinical features of fevers or pain, and no evidence of raised biochemical inflammatory markers.
Pulmonary embolism is a known surgical complication, due in part due to prolonged immobility [2]. It typically originates from lower limb DVT. Its occurrence following tonsillectomy was reported by Leonard et al. They describe the case of a 32-year-old patient who developed acute PE 36 h following tonsillectomy, in the setting of prolonged intubation and occult active malignancy [4]. In that case, the lower limb Doppler US failed to identify a DVT, and the source of the embolus was never identified.
The management of PE in the post-tonsillectomy patient is difficult due to the high risk of secondary haemorrhage. This is variably reported between 1 and 20% following tonsillectomy, but the likelihood is increased with therapeutic anticoagulation [1]. The use of an inferior vena cava (IVC) filter has been reported as an anticoagulant-sparing strategy in lower limb DVT, however, this is not effective in IJV thrombosis [2]. Careful monitoring of the anticoagulant therapeutic range is imperative to reduce bleeding risk. The authors advocate the use of an unfractionated heparin infusion, due to its reversibility and the ability to titrate the dose according to activated partial thromboplastin time (APTT) (Fig. 1).
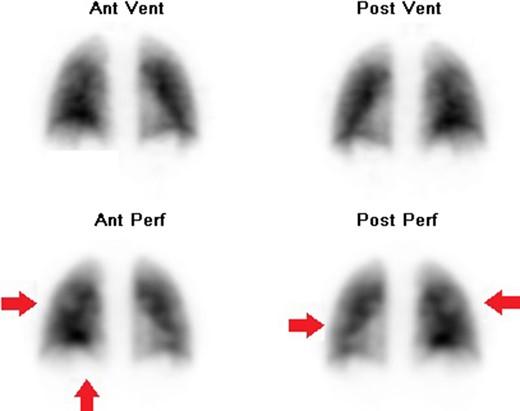
VQ scan showing bilateral ventilation perfusion mismatches, indicative of multiple pulmonary emboli. Ant = anterior; post = posterior; vent = ventilation; perf = perfusion.
CONCLUSION
Pulmonary embolism due to jugular vein thrombosis is a rare complication of tonsillectomy. The IJV should be considered as a potential source of thromboemboli in all patients who present with pleuritic chest pain following tonsillectomy or other head and neck surgical procedures.
ACKNOWLEDGEMENT
Mr Paul Yuen, for supervision of the clinical case without contribution to the case report.
CONFLICT OF INTEREST STATEMENT
The author declares that there is no conflict of interest regarding the publication of this article.
AUTHORSHIP STATEMENT
The single author prepared the entirety of the article. The article has been read and approved, and the author believes that the manuscript represents honest work.



