-
PDF
- Split View
-
Views
-
Cite
Cite
Amanda Brevilheri Benassi, João Paulo Fernandes Guerreiro, Alexandre de Oliveira Queiroz, Roberto Grange Gasparelli, Marcus Vinicius Danieli, Anterior and posterior cruciate ligament agenesis, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy216, https://doi.org/10.1093/jscr/rjy216
Close - Share Icon Share
Abstract
Congenital absence of the cruciate ligament is a rare condition with a prevalence of 0.017 per 1000 live births. This study reports a case of congenital absence of the anterior and posterior cruciate ligaments of the left knee associated to a type 1A fibular hemimelia, and a contribution to the existing hypotheses on knee ligaments development. According to medical literature the anomaly begins to develop around the seventh–eighth week of pregnancy. Patients with a cruciate ligament agenesis will often need a knee replacement at one point in their lives.
INTRODUCTION
Congenital absence of the anterior cruciate ligament (ACL) associated to posterior cruciate ligament (PCL) is a rare pathology. This condition has a prevalence of 0.017 per 1000 live births globally [1–3]. It is usually associated with other knee deformities, such as hypoplasia of the lateral femoral condyle, tibial intercondylar spines, absent or abnormal meniscus, congenital femur shortening, defects in the fibular head and its associated muscles as well as patellar dislocation [4].
The treatment of this condition remain an open debate among the authors and the opinions vary between the conservative and surgical treatments.
This is a case report of congenital absence of ACL and PCL associated with type 1 A fibular hemimelia.
CASE REPORT
A male patient presented with the history of late onset of walking at age 3 associated with low performance in sports practice. At age 12 the patient was diagnosed with limb size discrepancy whereby his affected left limb was 3.5 cm shorter than the right. Patient were treated with another surgeon in a different public hospital with an epiphysiodesis surgery at the time, successfully correcting the discrepancy. However, from the age of 8 the patient complained of instability of the affected knee and has begun to suffer from pain and repetitive sprains. Although the patient accessed several other services, a definitive treatment for this problem was not provided.
He was referred to this service at age 17, complaining of repetitive sprains, pain and joint locking. Physical examination showed that the patient experienced pain in the affected knee with range of motion of 5°–120°. His test for Anterior and Posterior Drawers as well as the Lachman, Pivot Shift, McMurray and Appley tests all showed positive results.
Radiographic images of the knees in AP (anteroposterior) and Lateral views and the panoramic of lower limbs (Fig. 1) were taken and confirmed a case of type 1 A fibular hemimelia on the affected side.
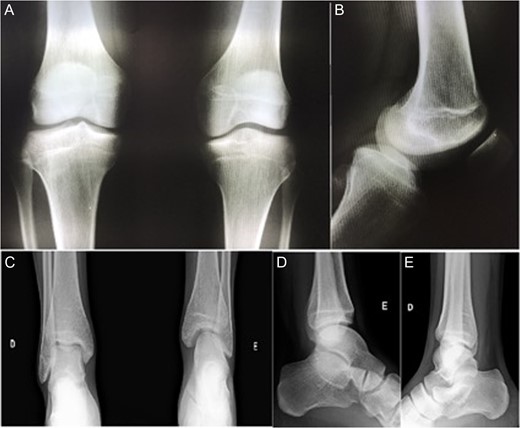
AP radiographic view of the knees (A) and lateral view of left knee—affected (B). AP (C) and lateral view (D and E) of the ankles. Note in (A) tibial spines hypoplasia of left knee, and in (C) left tibiotarsic joint dysplasia with fibular shortening, also noted in (D).
Magnetic resonance imaging (MRI) also showed bucket handle tear of the medial meniscus, complete absence of ACL and PCL, joint effusion, patellofemoral dysplasia, lateral patellar tilt and superficial patellar chondropathy (Fig. 2).
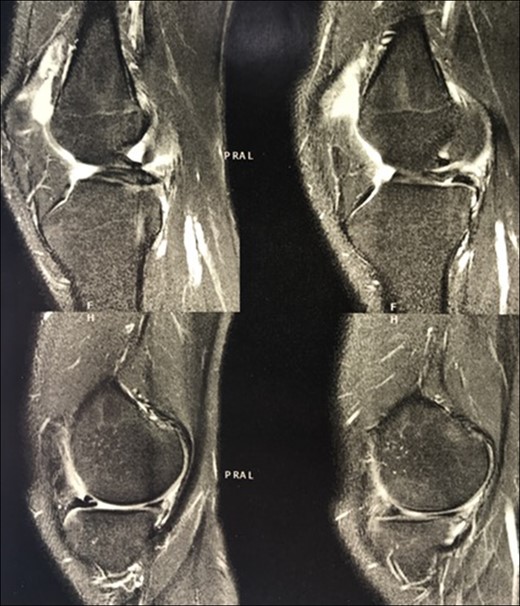
MRI of the affected knee showing the congenital absence of the cruciate ligaments (circles) and the presence of a bucket handle tear of the medial meniscus (arrow).
The patient underwent arthroscopic ACL reconstruction using ipsilateral flexor tendons as graft, PCL reconstruction using contralateral flexor tendons as graft and partial meniscectomy (Figs 3–5).
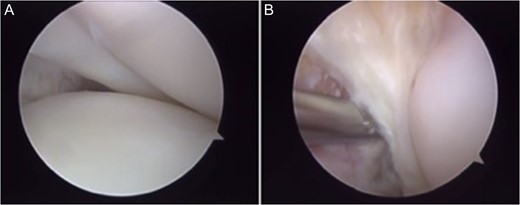
Arthroscopy surgery view during cruciate ligaments reconstruction. Note in (A) and (B) the ligaments absence. The lateral meniscus has not its bone tibial insertion of the posterior horn (*), which continued with the anterior meniscus femoral ligament (Humphry), which was hypertrophied (**). LFC, lateral femoral condyle.
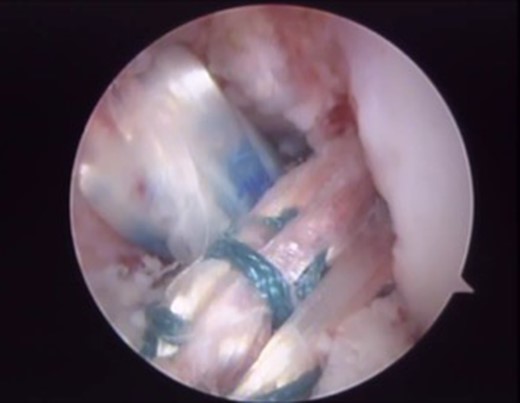
Final arthroscopic surgery image of the ACL and PCL reconstruction with the grafts tense and well positioned.
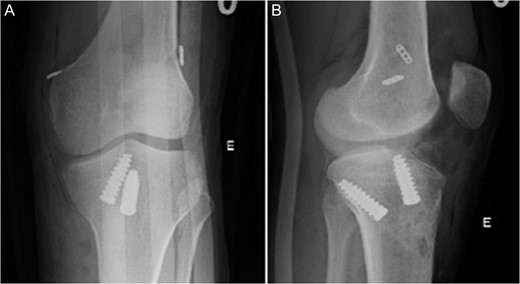
Radiographic image in AP (A) and lateral view (B) of left knee after surgery.
Patient was instructed to avoid weight bearing over the operated limb with a pair of crutches and use a non-hinged brace for 6 weeks after surgery, as well as to start physical therapy for muscle activation, patellar mobilization and range of motion gain. The patient was cleared for partial weight bearing at week 4 and full weight bearing at 8 weeks after the procedure. Six months after the surgery the patient reached 0°–120° of range of motion; tested negative on the Posterior Drawer, Pivot Shift, Appley and McMurray tests and grade 1+/4+ with firm endpoint on the Lachman and Anterior Drawer tests. He felt more stable when walking; was able to run and ride a bike. He chose not to return to contact sports to avoid further injuries. He continues to be monitored.
DISCUSSION
Congenital absence of the ACL and PCL together is a rare condition. The isolated congenital absence of ACL is a more common condition, whereas the absence of PCL is less prevalent and is usually associated with the absence of ACL, which indicates how extremely rare is this case. Such malformations are related to knee dislocation [5].
Manner et al. [2] classified three main types of dysplasia of the cruciate ligaments. Cases of hypoplastic or aplastic ACL and normal PCL are classified as Type I. Cases where the aplastic ACL is in combination with a hypoplastic PCL are Type II. When both cruciate ligaments are aplastic, as in the presented case, they are classified as Type III. Liu et al. [6] identified a genetically inherited autosomal dominant pattern responsible for the agenesis of ACL and PCL. This defect appears between the 7th and 10th weeks of intrauterine life when the intra-articular structures of the knee are formed [7].
Another finding of this case, already documented in medical literature, was the hypoplastic medial and lateral intercondylar tibial spines of the left knee of the patient, associated to fibular hemimelia [3]. This fact reinforces Giorgi’s hypothesis whereby the tubercles are formed due to the traction from the ACL, as the main function of the intercondylar tibial spines appears to be holding the cruciate ligaments [8]. This contradicts some authors who argue that dysplasias occurring in the knee are not consequences of each other, but rather separate events [2].
Another interesting detail noted in this case was the absence of the tibial bone insertion of the posterior horn of the lateral meniscus, which in this case was continued with a hypertrophied meniscal femoral ligament (Fig. 3). Perhaps an anatomical attempt to stabilize the knee, but without success.
Some authors still find the treatment approach of reconstructing the absent cruciate ligaments controversial. They argue that the absence of the cruciate ligaments is generally well tolerated, whereas reconstruction surgeries have had low success rates and poor functional results. Moreover, the joint surface in these cases could theoretically be able to adjust itself to compensate the distribution forces because of the absent ligaments [1]. However, other authors are in favour of ligament reconstruction [9, 10].
Despite these disputes, what seems inevitable for these patients is the progress towards a knee replacement.
CONFLICT OF INTEREST STATEMENT
None declared.



