-
PDF
- Split View
-
Views
-
Cite
Cite
Paul Welford, Håkan Alfredson, Achilles insertion bone pathology not related to pain in a triathlete with cystic fibrosis, Journal of Surgical Case Reports, Volume 2018, Issue 8, August 2018, rjy182, https://doi.org/10.1093/jscr/rjy182
Close - Share Icon Share
Abstract
This report concerns the unusual case of a 48-year old, world-class triathlete who has won 11 ironman competitions. She has reached the top level of international endurance sport in spite of being diagnosed with cystic fibrosis. This patient presented with Achilles pain and severe bony pathology at her left Achilles insertion. Traditionally this condition is treated via tendon detachment and re-attachment or intra-tendinous surgery, followed by a protracted rehabilitation. These procedures were considered risky due to this patient’s chronic disease with vulnerability to immobilization. Instead, she was treated by surgical removal of the superficial bursa alone, under local anaesthetic. This allowed the patient to become active and load her Achilles tendon immediately, and resulted in a significant symptomatic improvement. This case illustrates that despite the presence of severe tendon and bone pathology at the Achilles insertion, pain may originate in the superficial bursa; a structure ignored by traditional operations.
INTRODUCTION
This report illustrates the unusual case of a 48-year old, world-class triathlete who has won 11 ironman competitions. She suffers from cystic fibrosis (CF) yet has been successful in elite-level international endurance sport. She presented with Achilles pain and severe bony pathology at her left Achilles insertion that prevented her participation in sport.
CASE REPORT
The patient presented with a 6-year history of chronic left Achilles pain and reported a gradual worsening of her symptoms. Previous treatments included platelet-rich plasma injections but the patient described no lasting improvement. During the year leading up to surgery, her left Achilles pain prevented her from running on consecutive days. At the time of her surgery, she had not competed for 4 months, and was unable to tolerate footwear with a closed heel and experienced severe pain on a daily basis.
VISA-A was used before surgery and at follow up. This validated questionnaire provides an index of severity when assessing Achilles’ tendinopathy severity, and is widely used in both research and clinical practice [1]. Preoperative VISA-A score was 25/100.
Past medical history included CF, diagnosed at age 20. Daily medications included salbutamol and budesonide inhalers and hypertonic saline inhalation. She was previously treated with ciprofloxacin for persistent pseudomonas infection and had recently taken doxycycline and azithromycin for respiratory infection. She undertakes daily aerobic exercise to manage her condition.
The patient had previously consulted an orthopaedic specialist, who offered surgery. The proposed operation was Achilles detachment and removal of bone pathology, followed by tendon re-attachment. This procedure requires a long period of rehabilitation that begins with a non-weight bearing phase, and progresses to partial loading [2]. The patient was concerned that this relative immobility might be detrimental both to the management of her CF and to her career as an athlete, leading her to seek alternative options.
On examination, there was thickening and localized tenderness over the left subcutaneous bursa and a slightly widened heel profile. The distal Achilles was thickened. There was no tenderness or swelling in the region of the retrocalcaneal bursa, nor any thickening or tenderness over the tendon midportion.
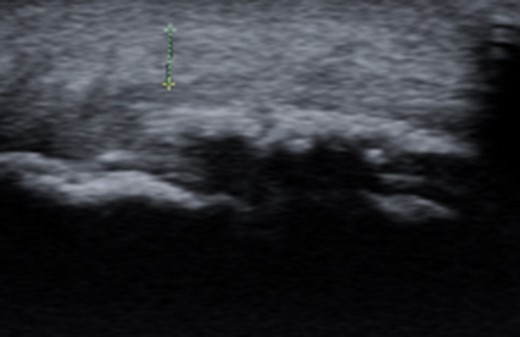
Dynamic ultrasound examination of the left heel showed a diffusely thickened subcutaneous bursa, with fluid-rich islands. Regions of high blood flow were seen in the bursal walls. There was tendinopathy in the distal Achilles, which measured 6–7 mm in thickness with intra-tendinous bone formations and calcification, but no high blood flow. Finally, there was a minor Haglund-like deformity with a sharp edge and a slightly enlarged retrocalcaneal bursa with the appearances of scar tissue formation, but no fluid or increased blood flow. There were no signs of partial ruptures in the distal part of the Achilles. These ultrasound findings were consistent with those of a previous MRI (Figs 1–5).

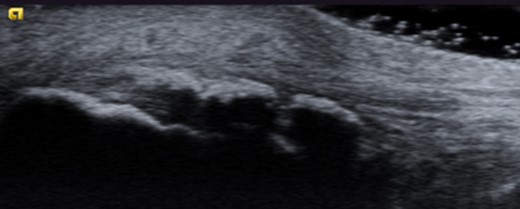
Ultrasound image of thickened subcutaneous bursa and bone formations in the distal Achilles.
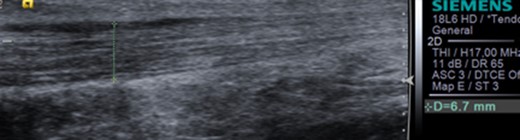
Ultrasound image of diffusely thickened subcutaneous bursa and underlying intra-tendinous bone formations.
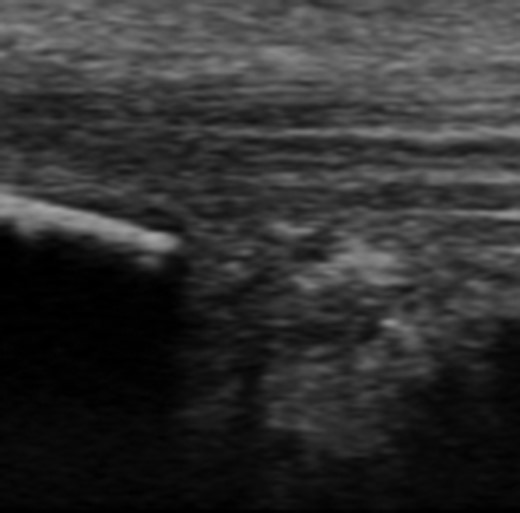
Ultrasound image of minor Haglund deformity with sharp edge. Enlarged retrocalcaneal bursa with appearance of bursal scar tissue formation.
Provocation testing followed, via 5 min of painful skipping and running. Ultrasound appearances were unchanged after provocation. At this point, an ultrasound-guided injection of local anaesthetic was delivered into the subcutaneous bursa. Following this diagnostic injection, further provocation tests were administered. These tests, which included running and skipping on tip-toe, were completely pain free.
The diagnosis was chronic insertional Achilles tendinopathy with bursa and bone pathology. More specifically, findings suggested that the subcutaneous bursa was this patient’s main source of pain.
Plans were made to surgically remove the subcutaneous bursa and explore the superficial surface of the distal Achilles tendon under local anaesthesia. If partial rupture was excluded, treatment would consist of bursal excision only.
Operation commenced with a longitudinal excision on the lateral aspect of the Achilles. The subcutaneous bursa was found to be thickened and richly vascularised. This was carefully released from the skin and tendon before being removed. In regions, the bursa was completely coalesced with the tendon, with islands of fatty infiltration. There were no partial ruptures on the superficial aspect of the distal Achilles. Haemostasis was established and flush was administered before closure.
Postoperative rehabilitation commenced with rest, elevation and mobilization. The patient was reviewed on Day 2: Wound inspection was satisfactory, with no swelling or bleeding. On ultrasound examination, there was only minor haematoma and no change to tendon appearances. The patient was permitted to fully weight bear in an open-heeled shoe from Day 2. Walking distances gradually increased, with eccentric training from tiptoe position to floor level and light jogging starting at week 7.
This patient was followed up continuously via e-mail. At 7-month follow up, she reported being pain-free and having recently run a 10 km race in 38 min. At 2-year follow up, the patient’s VISA-A score was 81 and she had successfully completed a marathon. She reported being completely free of pain over the preceding 6 weeks and able to walk normally after running 33 km.
DISCUSSION
Traditional operations for insertional Achilles tendinopathy do not involve removal of the subcutaneous bursa [3]. This patient had previously been offered surgical removal of intra-tendinous calcifications, followed by tendon reinsertion with bone anchors. Maffulli published longitudinal results from this procedure in 2004. Of the 21 patients operated, 11 reported an ‘excellent’ outcome, while five had a ‘good’ result. The remaining five patients were unable to return to their previous level of sport [2]. There is, to our knowledge, no literature describing isolated excision of the subcutaneous bursa.
An anatomical study by Andersson et al. [3] offers a possible explanation for this patient’s pain relief following bursal excision. Immunohistochemical staining techniques were used to analyse nerve distributions in specimens from 10 patients undergoing surgery for insertional Achilles tendinopathy with ultrasound verified pathology in the distal Achilles, subcutaneous and retrocalcaneal bursae and Haglund deformity. The authors examined the three tissues that are traditionally considered to be involved in this pathology; bony Haglund deformity; Achilles tendon and retrocalcaneal bursa. In addition, the nerve supply to the subcutaneous bursa was analysed. Of the four tissues studied, the subcutaneous bursa was found to be by far the most densely innervated, raising the possibility that this may be an important and overlooked pain causing structure in insertional Achilles tendinopathy.
CONFLICT OF INTEREST STATEMENT
None declared.



