-
PDF
- Split View
-
Views
-
Cite
Cite
Melissa M Levack, Amy G Fiedler, Haytham Kaafarani, David R King, Perforation of a mesenteric Meckel’s diverticulum, Journal of Surgical Case Reports, Volume 2018, Issue 6, June 2018, rjy126, https://doi.org/10.1093/jscr/rjy126
Close - Share Icon Share
Abstract
Meckel’s diverticulum is a remnant of the embryologic omphalomeseteric duct and is a common congenital anomaly found in ~2% of the population. The clinical significance of this anomaly is that the persistent diverticulum can lead to intestinal obstruction or diverticulitis and may contain ectopic tissue which can lead to bleeding, ulceration or perforation. The classic location of a Meckel’s diverticulum has been described ~40 cm from the ileocecal valve on the antimesenteric side of the distal ileum. There have only been a few documented cases of a Meckel’s diverticulum found on the mesenteric border of the ileum. In this report, we describe a patient who presented with a perforated Meckel’s diverticulum which was found on the mesenteric border and performed a review to determine the significance of this finding.
INTRODUCTION
In 1809, Johann Friedrick Meckel described the embryological phenomena which occurs when the vitelline duct fails to involute leaving behind a structure known as Meckel’s diverticulum. Classic diagnostic criteria for a Meckel’s diverticulum dictate that the structure contains all five layers of small intestine, have a separate mesentery for blood supply, arise from the antimesenteric border of the ileum and be located ~40 cm proximal to the ileocecal valve. Despite these criteria, there are only a handful of cases [1–5] which challenge the diagnostic concept that a Meckel’s diverticulum must arise from the antimesenteric border. We present a patient who was treated for a perforated Meckel’s diverticulum found on the mesenteric border.
CASE REPORT
A 27-year-old male presented to the Emergency Department 5 h after the onset of severe right sided abdominal pain. He was afebrile, normotensive with a normal heart rate. He denied any other associated symptoms. His exam was notable for a soft abdomen which was tender to palpation in the right lower quadrant with associated voluntary and involuntary guarding. He had a Rovsings and obturator sign. His white blood cell count was 13 with 79% polys. A CT scan of the pelvis with rectal contrast was obtained. The diagnostic interpretation was acute appendicitis with likely perforation. The appendix was reported to be dilated, measuring 9 mm in diameter with associated wall thickening, surrounding fat stranding and hyperemia. Fluid was noted in Morrison’s pouch, along the paracolic gutter and in the pelvis (Fig. 1). The decision was made to proceed to the operating room for a laparoscopic appendectomy.
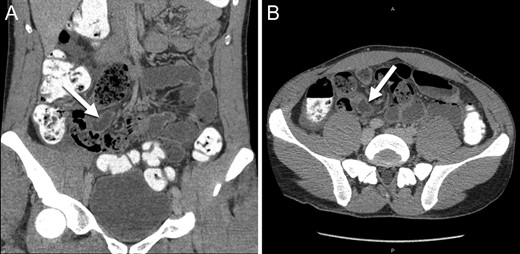
Abdominal CT scan ((A) coronal and (B) axial slices) showing a dilated and inflamed tubular structure indicated by the white arrows misinterpreted as acute appendicitis.
An infraumbilical skin incision was made and a Hasson trocar was placed under direct visualization. Once adequate pneumoperitoneum was established, a 5 mm camera was inserted through the umbilical port. Two additional 5 mm trocars were placed, one in the suprapubic region and one in the left lower quadrant. The small bowel was mobilized and there was a significant amount of purulence. The cecum was bluntly mobilized, however, an inflamed appendix was not visualized. The remainder of the abdomen was inspected. There was a structure protruding from the mesenteric side of the distal ileum which had an obvious perforation at the base and nearby abscess cavity. This structure was felt to be most consistent with a perforated Meckel’s diverticulum although the location was unusual. In order to perform an appropriate excision, a small midline incision was made for small bowel resection. This was completed with a stapled anastomosis. Intra-operative frozen section of the pathologic specimen revealed a bowel diverticulum with gastric mucosa (Fig. 2). The abdominal cavity was then irrigated and the patient was closed in standard fashion. Post-operatively, his recovery was uneventful. He was discharged on post-operative Day 2 and was seen two weeks later without further symptoms. Final pathology confirmed a 5.0 cm long diverticulum communicating with the small bowel containing both gastric body/fundic-type mucosa and pancreatic tissue in the diverticular portion of the specimen. Retrospective questioning of the patient revealed that he had a previous 6-month period of intermittent bloody stools and was referred to have a colonoscopy but never followed up.
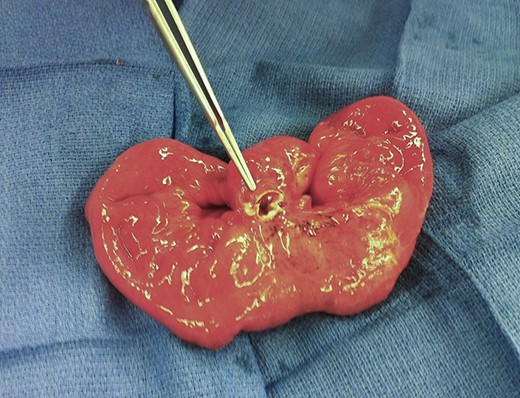
Intra-operative picture of the surgical specimen depicting the mesenteric-sided Meckel’s diverticulum with a clear perforation at the base of the diverticulum.
DISCUSSION
Embryologic omphalomeseteric duct anomalies are found in ~2% of the population due to failure of absorption of the vitelline duct. In addition to persistence of the duct, such anomalies may also be associated with mesodivertocular bands which are thought to be remnants of a persistent left vitelline artery. In 1941, Chaffin first described a case of an inflammatory mass located on the mesenteric surface of the ileum [1]. The atypical location of the structure prompted the authors to consider alternative diagnoses such as an enterogeneous cyst, however, they thought it was most consistent with an unusual variant of a Meckel’s diverticulum. Segal et al. [2] published a report describing a patient operated on for appendicitis who was found to have an inflammatory mass originating from the mesenteric border of the ileum proximal to the ileocecal valve. While the presence of gastric mucosa in the mass could not exonerate the diagnosis of an enterogenous cyst, the authors could not conclude with certainty if this was a duplication cyst or atypical Meckel’s diverticulum with an obliterated lumen due to inflammation. Sarioglu-Buke et al. [3] describe a boy who was operated on for painless rectal bleeding and work-up revealed a Meckel’s diverticulum on the mesenteric surface directly communicating with the ileum. Additionally, the diverticulum was noted to have its own blood supply in contrast to ileal duplication cysts which share the wall and blood supply of the ileum. In our patient, there was a clear communication with the intestinal lumen as well as a fat pedicle containing a vascular supply directly to the diverticulum exonerating the concept of an enterogenous or duplication cyst and further supporting the diagnosis of this atypical variant.
A Meckel’s diverticulum may lead to intestinal obstruction or diverticulitis and can contain ectopic tissue which leads to bleeding, ulceration or perforation. The abnormal location of the diverticulum on the mesenteric border raises concerns that this variant may be more likely to rupture or erode into the mesentery placing the patient at risk for bleeding or more serious complications. Although this has not definitively been proven, it does raise an interesting question about the operative management of these diverticuli when identified. We recommend that in symptomatic patients, the diverticulum be removed either via an open or laparoscopic approach if feasible [6] with either a diverticulectomy or small bowel resection. In incidental cases, a diverticulectomy should be performed if the patient is undergoing surgery for other reasons.
In summary, despite the ‘classical’ description, Meckel’s diverticula may be located on the mesenteric boarder. The diagnosis of a perforated Meckel’s diverticulum can often be missed on radiographic imaging and the surgeon should have a high clinical suspicion of this pathology if the appendix appears normal. Finally, the finding of an incidental mesenteric Meckel’s should prompt consideration for resection given the propensity for perforation or inflammation and the proximity to nearby vasculature.
Conflict of Interest statement
None declared.



