-
PDF
- Split View
-
Views
-
Cite
Cite
Basmah A Rafie, Omar J AbuHamdan, Nawal S Trengganu, Badr H Althebyani, Bassam S Almatrafi, Torsion of a wandering spleen as a cause of portal hypertension and mesenteric varices: a rare aetiology, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy107, https://doi.org/10.1093/jscr/rjy107
Close - Share Icon Share
Abstract
A wandering spleen is a condition characterized by excessive splenic mobility due to the mal-development or the laxity of its ligaments that leads to migration from its normal anatomical location. This condition renders its long mobile vascular pedicle liable to torsion and occasional infarction. Herein, we report a case of a 27-year-old nulliparous woman who presented with acute abdominal pain and a tender right-sided pelvi-abdominal mass. CT scan of the abdomen and pelvis revealed a torted, infarcted wandering spleen with portal hypertension and mesenteric varices that mandated an emergency splenectomy. Although there are a few reported cases describing the association of wandering spleen with portal hypertension and fundal varices, cases of mesenteric varices are extremely rare. To the best of our knowledge, this case is considered the third reported case of a wandering spleen which was subsequently complicated by portal hypertension and mesenteric varices that was managed effectively with splenectomy.
INTRODUCTION
A wandering spleen, which is also known as an ‘ectopic spleen’, is a rare condition caused by the improper development or weakening of the ligaments that hold the spleen stationary. (The congenital mal-development of the dorsal mesogastrium or the acquired laxities of its ligaments are the possible causes of this condition). Thereby, the spleen is attached at the hilum by only a long vascular pedicle and the organ ‘wanders’ in the lower abdomen or pelvis where it may be mistaken for an unidentified abdominal mass. This extra-anatomical ‘ectopic’ position in the abdomen or pelvis (depending on the length of its vascular pedicle) contributes to its variation in clinical presentations and makes the diagnosis and management challenging [1].
Despite the increasing rate of similar reports in medical literature, the actual worldwide incidence is still unknown. It is characterized by a bimodal incidence as it generally manifests in children and in the third decade of life [2].
The aim of this report is to share our experience about the presenting features, and the pitfalls encountered in the management of such rare condition.
CASE REPORT
A healthy 27-year-old nulliparous woman reported to the emergency department with a 2-day history of upper abdominal pain associated with repeated vomiting and constipation.
Her symptoms had developed gradually over 2 years prior to her presentation. She used to experience frequent episodes of upper abdominal pain (mainly in the epigastrium radiating to both hypochondria) and this pain was relieved by placing herself laterally on either sides of the abdomen during the attacks. The bouts of pain were associated with occasional episodes of vomiting but she had never presented herself to the emergency department. A few months prior to her presentation to the hospital, the attacks of pain increased and became more frequent. On the day of her admission, the intensity of pain had increased to the extent of interfering with her movements and activity. The patient had never experienced any abdominal trauma or had never undergone any abdominal surgeries.
Upon admission, her vital signs were blood pressure of 105/61 mmHg, a pulse rate of 86 beats/min, and there was no evidence of fever. An abdominal examination revealed a tender right-sided pelvi-abdominal mass. A digital rectal examination was unremarkable.
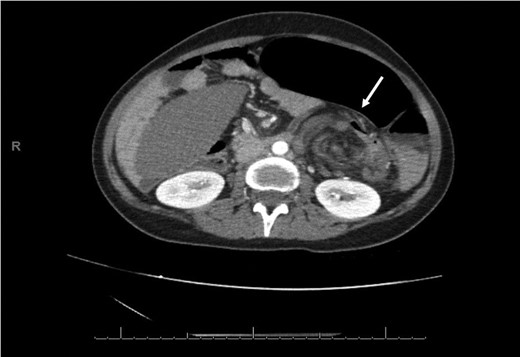
Laboratory investigation showed a white blood cell count of 15.13 × 103/UL, (mainly neutrophilia of 90.3%), a hemoglobin level of 9.4 g/dL, and a platelet count of 189 × 103/UL. The other biochemical parameters including liver enzymes were normal apart from a trace of jaundice, with total Bilirubin of 2.43 mg/dL and direct Bilirubin of 0.45 mg/dL. Chest X-ray showed bowel loops at the splenic fossa (Fig. 1). An initial diagnosis of a torted ovarian cyst was made. A pelvi-abdominal ultrasound revealed normal adnexa but a right-sided soft pelvic-abdominal mass with the absence of a splenic shadow at the left hypochondrium. Subsequently, CT scan of the abdomen and pelvis revealed a large right-sided infarcted spleen of 30 × 16 × 10 cm3 (Fig. 2) and a ‘whirl sign’ of the splenic pedicle (Fig. 3). Furthermore, CT scan showed signs of portal hypertension (Fig. 4) associated with mesenteric varices (Fig. 5). The patient subsequently underwent a surgical exploration.
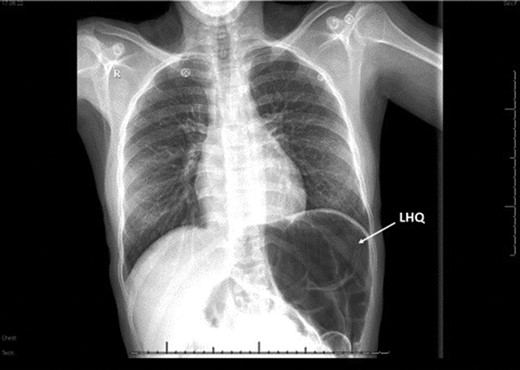
Chest x-rays; absence of gastric bubbles at the left hypochondria (LHQ; white arrow) that was replaced with bowel loops.

Computed tomography of the abdomen and pelvis with IV contrast shows a non-enhancing (infarcted) spleen (dotted arrow) that has completely migrated to the right side of the abdomen and pelvis.
An axial CT of the upper level of the abdomen shows a corkscrew-like soft tissue density (white arrow) indicating twisted splenic vessels surrounded by peritoneal ligaments and fats forming a whirly appearance with alterative lucent and dense bands (a whirl sign), is a pathognomonic CT findings of torsion.
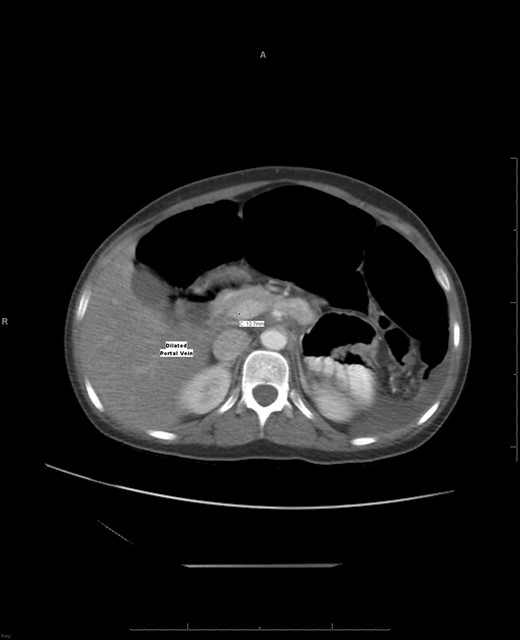
An axial CT shows a widening portal vein 12.7 mm in diameter indicating portal hypertension with multiple dilated portal veins seen at the liver parenchyma.
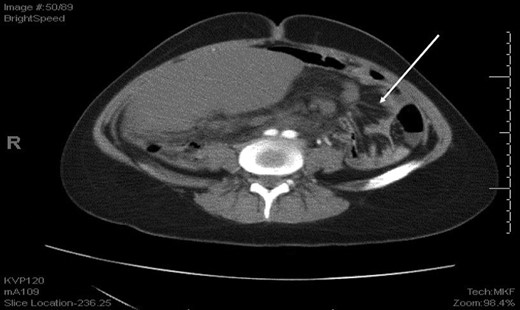
An axial CT shows dilated engorged mesenteric vessels (white arrow) indicating mesenteric varices.
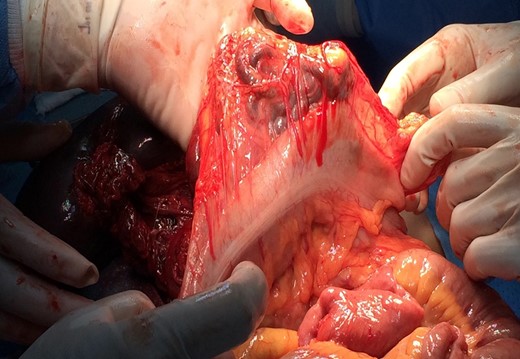
An exploratory Laparotomy through a midline incision revealed that the spleen was infarcted and torted around its long vascular pedicle in a 1980° clockwise rotation (11 twists), for which an emergency splenectomy was performed (Fig. 6). In addition, conservative management was elected for the abnormally dilated and tortuous veins that surrounded the splenic pedicle and the greater curvature of the stomach (Fig. 7). However, 6 h postoperatively, the patient was taken for re-exploration due to bleeding from these tributaries for which devascularisation and ligation of all tributaries was performed until hemostasis was secured.

Intraoperative view of an infarcted wandering spleen with a whirly appearance of splenic pedicles surrounded by peritoneal ligaments and fats.
Intraoperative view of dilated tortious tributaries of the superior mesenteric vein adjacent to the handled transverse colon.
Apart from paralytic ileus which was managed conservatively, she was on broad spectrum antibiotic and discharged on the 10th postoperative day in a good condition after she received prophylactic triple vaccine against Haemophilus influenza, Pneumococcus and Meningococcus. Furthermore, she continued the prophylactic antibiotic for 1 month postoperatively. Currently, she is in the third year of her follow up, displaying good health and underwent a laparoscopic cholecystectomy for cholelithiasis with an uneventful recovery.
DISCUSSION
A broad description of clinical manifestation of wandering spleen has been found in the literature. It varies from asymptomatic, incidentally discovered conditions such as spontaneous atraumatic rupture [3] or a palpable mass to different degrees of abdominal pain due to acute, subacute, and chronic torsion and detorsion of its vascular pedicle [4, 5]. Furthermore, the reported degree of torsion ranges from 90° (1/4 twist) to 2160° (12 twists) depending on its length and mobility [6].
A wandering spleen can be complicated by hypersplenism, splenic infarction, portal hypertension and/or varices. Although a few cases of a wandering spleen complicated by the fundal varices and left sided portal (sinistrial) hypertension have been reported, but complications of mesenteric varices are considered rare [7]. To the best of our knowledge, this is the third reported case after two cases reported by Zarroug et al. [8] of a wandering spleen complicated by the mesenteric varices; both were managed successfully by splenectomy.
The authors concluded that, in this case the most likely mechanism of portal hypertension with mesenteric varices in absence of portal vein thrombosis is the mechanical occlusion of extrahepatic portal vein at the level of superior mesenteric and splenic vein confluence due to splenic torsion and its migration to the right side of the abdomen. Subsequently, this led to retrograde long-standing vascular congestion, splenic vein occlusion, and eventually its infarction along with portal hypertension and mesenteric varices.
As the diagnosis of torsion of a wandering spleen is challenging, CT scan imaging showing the characteristic sign of a ‘whirled appearance’ of the splenic pedicle is considered the preferred modality for diagnosis of this condition [9].
Management of splenic torsion evolved at the beginning of 20th century, primarily from ‘a splenectomy approach’ toward ‘splenopexies’ using laparoscopic techniques. Currently, splenopexy is the standard surgical procedure for the management of a wandering spleen if it is not infarcted [10]. However, if the patient develops complications such as those described above, a splenectomy may aid in the elimination of varices in addition to symptomatic relief and the subsequent prevention of any relapse [7, 8].
In conclusion, torsion of a wandering spleen is considered a life-threatening emergency. Therefore, early recognition and prompt surgical intervention in symptomatic cases aiming at preservation of the spleen whenever possible is the primary goal in managing such conditions.
CONFLICT OF INTEREST STATEMENT
The authors declare that we have no conflicting interest, and have not been supported, or funded by any drug company.
FUNDING
The authors declare that there was no funding or grant support in this scenario.
PATIENT CONSENT
Consent for taking intraoperative photographs was obtained before the patient’s initial operation.



