-
PDF
- Split View
-
Views
-
Cite
Cite
Haneen Al-Maghrabi, Abdelrazak Meliti, Primary bilateral ovarian Burkitt lymphoma; a rare issue in gynecologic oncology, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy113, https://doi.org/10.1093/jscr/rjy113
Close - Share Icon Share
Abstract
We report a rare case of 42-year-old female patient with bilateral primary ovarian Burkitt lymphoma (BL). Primary BLs are rare ovarian oncology neoplasms. Only few cases are reported in English literature, most of them are presented in pediatric and young adult age groups. Rare cases are reported in adult females. Although BL is a rare primary ovarian neoplasm, it is very important to establish an accurate diagnosis as early as possible for therapeutic purposes.
INTRODUCTION
In 1958, Dennis Burkitt, a British surgeon, described a childhood tumor while working in Uganda characteristically occurs among African children. Back then, the tumors appeared to be limited to the warm wet tropics of Africa and Papua New Guinea [1]. Burkitt lymphoma (BL) is a malignant non-Hodgkin lymphoma associated with c-MYC gene translocation and heavy locus immunoglobulin, resulting in the most common variant translocation t (8;14) (q24;q32). BL commonly occurs in childhood age group; nevertheless, it is a rare presentation in adults as compared to low-grade B-cell lymphomas, diffuse large B-cell lymphoma. The World Health Organization (WHO) classification of lymphoid neoplasms sustained the BL subtypes into three subtypes as follows: endemic BL, sporadic BL and immunodeficiency-associated BL [2]. The endemic BL is characteristically associated with Epstein–Barr virus (EBV) infection. Sporadic BL occurs in the second and third decades of life, commonly in Western Europe and North America, can involve extra-nodal sites such as intestinal tract, mesentery, and more commonly at the ileocecal junction. The latter is frequently seen in the pediatric population probably due to high lymphoid tissue compartment in this area [3]. Immunodeficiency-associated BL mostly detected in patients with primary immunodeficiency, HIV, and post organ transplant [3]. BL seen commonly in boys with average ratio male: female (1.3:1). The average age at presentation is 8 years old (range: 0–20 years) [3]. Overall, primary bilateral BL is a rare diagnosis in adults. In this article we present a rare case of bilateral primary ovarian BL with its histopathology, immunohistochemistry and FISH analysis.
CASE PRESENTATION
A 42-year-old lady presented to the emergency department at our hospital complaining of continuous abdominal pain and a palpable abdominal mass. No associated symptoms were identified. Physical examination demonstrated tender enlarged abdomen. Her blood work was unremarkable, except for high platelet level (480 × 109/L). Abdominal and pelvic computed tomography (CT) scan with oral and IV contrast revealed large bilateral lobulated soft tissue heterogeneous adnexal masses with some cystic components. There was an evidence of vascular enhancement within both adnexal masses. The largest mass (9.2 × 11.4 cm2). No radiological evidence of cystic rupture or hemorrhage were seen within both masses. The uterus was displaced by both adnexal masses. Both ovaries could not be visualized (Fig. 1A). Bone marrow aspirate showed mild increase in megakaryocytes with no evidence of infiltrative process. Chest x-ray and brain MRI scan were unremarkable for pathologic findings.
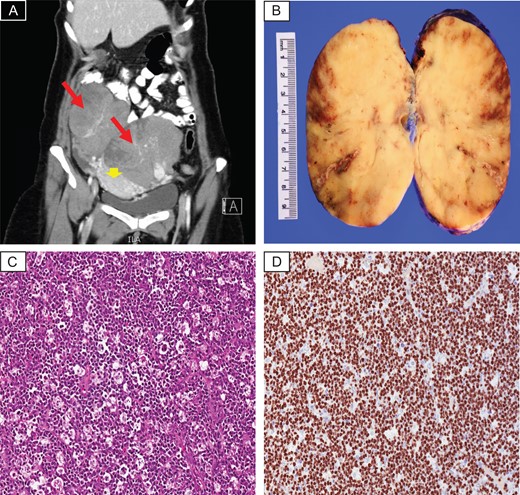
(A) CT scan with contrast revealed large bilateral lobulated heterogeneous adnexal masses (red arrows), displacing the uterus down (arrow head). (B) Gross photo showing homogenous white tan cut surface, focal areas of hemorrhage and necrosis are seen. (C) Histopathology examination demonstrates sheets of diffuse lymphoid infiltrate with prominent starry-sky appearance (H&E; ×20). (D) Ki67 proliferative index is almost 100% (×20).
The patient underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy. The specimen sent for pathologic evaluation. We received two separate adnexal masses, the right adnexal tissue composed of a single solid capsulated mass with smooth tan lobulated cut surface weighing 564 g and measuring 12 × 10 × 6 cm3. The left adnexal tissue composed of a single solid mass weighing 1040 g and measuring 15 × 10 × 7 cm3, with homogenous white tan lobulated cut surface, focal areas of hemorrhage and necrosis were seen (Fig. 1B). Microscopic examination of the sections taken from both masses revealed sheets of diffuse lymphoid infiltrate composed of medium sized lymphoid cells with minimal amphophilic cytoplasm, prominent basophilic nucleoli, coarse chromatin and thick nuclear membrane. Prominent starry sky pattern with numerous mitosis and apoptosis seen (Fig. 1C). By immunohistochemistry, the tumor cells revealed positive immunoreactivity against CD79a, CD20, PAX-5, CD10, BCL6 while negative for BCL2, CD3, CD5, CD21, CD23, CD1a, TdT and Cyclin D1. Ki67 proliferative index of 100% expressed in the tumor cells (Fig. 1D). Flow study result showed small lymphoid population expressing CD19, CD20, CD22 and CD10. In the meantime, FISH interpretation revealed positive BCL6 rearrangement and c-MYC (8q24) rearrangement. IGH/BCL2 [t (14; 18)] rearrangement was not detected. All of the above ancillary studies were consistent with the diagnosis BL. The patient planned to be treated with multi-agent chemotherapy R-CODOX and R-IVAC chemotherapy. Our patient currently is on her third cycle, doing well and alive.
DISCUSSION
Primary ovarian lymphoma (POL) is defined as a lymphoma that originates in the ovary and lacks other manifestations of lymphoproliferative disorders elsewhere. POL is a very rare entity in ovary due to absence of lymphoid tissue within the ovary. Primary ovarian non-Hodgkin’s lymphoma accounts only for 0.5 and 1.5% of all ovarian neoplasms. A number of theories looked at the pathogenesis and the origin of POL, some of them suggested that it originates from the lymphocytes surrounding the blood vessels in the hilum, and those near the corpus luteum [4]. Others claim it’s the reactive lymphocytes secondarily involved in the inflammatory response related to pelvic inflammatory disease, endometriosis, or autoimmune disease that undergo a malignant transformation. There’s only 50 cases reported of primary non-Hodgkin lymphoma, 21 are cases confirmed histopathologically as primary BL with average age 6–62-year-old (mean age 27.6 years).
Ovarian involvement by lymphoma can be primary or secondary. The secondary involvement either as an early metastasis in occult extra-ovarian neoplasms, or as a generalized metastatic diseases [5]. In 1988, Fox et al. [6] and Skodras et al. [7] suggested a diagnostic criteria for POL as follows: (i) lymphoma should be clinically confined to the ovary, adjacent lymph nodes or adjacent ovarian structure caused by direct spread, (ii) preoperative work up like bone marrow aspiration and peripheral blood smear should be negative, and (iii) metastatic lymphoma should appear at least months after primary ovarian involvement (Paladugu et al. [8] suggested 60 months after the diagnosis established). Top differential diagnoses of BL in adults would include diffuse large B-cell lymphoma, follicular lymphoma, small cell carcinoma, adult granulosa cell tumor and dysgerminoma. Histopathology examination stained by hematoxylin and eosin stain (H&E), and immunohistochemistry studies will show the characteristic features of BL. All of these findings were typically expressed in our case as described previously. All types of BL show translocation between c-MYC oncogene on chromosome 8 and one of the immunoglobulin genes, commonly the heavy chain gene on chromosome 14. Less commonly the κ light chain gene on chromosome 2 or the λ light chain gene on chromosome 22 [9].
It is very important to differentiate primary from secondary ovarian lymphomas. The prognosis and the survival rate of POL are variable depending on the stage at diagnosis. A 5-year survival rate in POL is 80%, while secondary cases are only 33% [10]. POL have a better survival rate probably due to the early presentation and early stage at diagnosis. The treatment depends on the risk-adapted approach by classifying the patients into high-risk and low-risk groups depending on the following criteria: tumor size (less or more than 10 cm), disease stage (bone marrow involvement and CNS infiltration), patient performance status, and lactate dehydrogenase level. Multi-agent chemotherapy is considered to be the most suitable therapeutic option for patients with BL.
CONCLUSION
In conclusion, we present a unique case of bilateral primary ovarian BL in a 42-year-old lady confirmed histologically and cytogenetically. Early diagnosis and therapy of BL is associated with better prognosis and survival rate.
Conflict of Interest statement
None declared.



