-
PDF
- Split View
-
Views
-
Cite
Cite
Rémy Liechti, Lana Fourie, Stefan Fischli, Jürg Metzger, Symptomatic lymphangioma of the adrenal gland: a case report, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy106, https://doi.org/10.1093/jscr/rjy106
Close - Share Icon Share
Abstract
Lymphangiomas (LAs) are rare benign tumors of the lymphatic vessels. In total, 95% of all reported LAs are located in the head, neck and the mediastinum. LAs of the adrenal gland are very rare and currently, only ~54 cases have been reported in literature. We present a case of a big left-sided adrenal LA. Abdominal imaging revealed a big cystic lesion in the left upper abdomen of unknown origin. For diagnostic and therapeutic reasons we performed explorative midline laparotomy. The left adrenal gland was found to be the origin of the cystic tumor. Hence, the patient underwent adrenalectomy in order to remove the intact cystic lesion. Diagnosis was then confirmed by histological examination. With adrenal LAs being a very rare entity, diagnosis is challenging and only little evidence exists on treatment options. We discuss diagnostic, therapeutic and surgical approaches concerning such cases and provide an overview of the current literature.
INTRODUCTION
Lymphangiomas (LAs) are rare benign tumors of the lymphatic vessels. The etiology of LAs has not yet been clearly established. They are believed to result from malformations of sequestered lymphatic tissue. These lesions can be present at birth or occur at any age. The most common sites of occurrence are head, neck and the mediastinum accounting for 95% of all reported LAs [1]. The remaining 5% are located in the abdominal cavitiy, involving the mesentery of the small intestine, mesocolon, omentum, pancreas or adrenal gland. LAs of the adrenal gland are very rare and currently, only approximately 54 cases have been reported in literature [2, 3]. These lesions are usually detected as asymptomatic, incidental finding in patients undergoing an abdominal imaging procedure for other reasons. The diagnosis is very challenging and to date, the histological tissue analysis remains the only reliable tool to confirm the diagnosis of an adrenal LA.
We present a case of a big left-sided adrenal LA causing non-specific abdominal pain and symptoms.
CASE REPORT
A 32-year-old female patient was referred to our emergency department complaining of progressive, colicky abdominal pain accompanied by intermittent nausea and vomiting during a period of more than 3 weeks. The pain was localized in the epigastric region and radiated through to the back. In addition, the patient complained of generalized paresthesia as well as episodes of hot flashes and palpitations. There was no alteration in stool consistency or frequency. Her past medical history revealed no long-term medication or previous abdominal operations.
On physical examination, the patient had normal vital signs. Her abdomen was soft, non-tender and non-distended. Laboratory investigations showed a slightly elevated white blood cell count as well as C-reactive protein level. Beta-HCG test was negative. Computed tomography scanning of the pulmonary arteries was performed in order to rule out pulmonary embolism. The simultaneous display of the upper abdomen revealed a big cystic lesion, which seemed to be attached to the left kidney. Biochemical analysis and hormone testing showed no signs of a hyper functioning mass. Abdominal MRI revealed a maximum diameter of 12.5 cm. The origin of the cystic lesion was suspected either in the mesentery or the omentum majus (Fig. 1A and B). Considering the abdominal symptoms as well as the fact that neither origin nor dignity could be determined in this patient, a total surgical removal followed by histological examination was indicated.
We performed an upper midline laparotomy. To ensure a good anatomical overview, mobilization of the left colonic flexure was necessary and the omental bursa was entered. The distal part of the pancreas showed close proximity to the cystic lesion and needed careful separation. After adhesiolysis between the splenic surface, the posterior gastric wall as well as the parietal peritoneum, the left adrenal gland with its associated vein, was found to be the origin of the cystic tumor. Hence total adrenalectomy was performed in order to remove the intact cystic lesion (Fig. 1C and D). Following a short period of postoperative nausea and vomiting, gradual return to a normal diet was possible. The patient was discharged on the sixth postoperative day.
The histological examination of the specimen revealed an adrenal lymphangioma located in a normal structured adrenal gland.
At the 3-month follow-up, the patient presented with sleep disorder, nausea and weight loss. The ACTH stimulation test showed a relative adrenocortical insufficiency while DHEA-S levels remained normal. Consecutively the patient was treated with hydrocortisone, as needed during stressful situations. The further course remained uneventful (Fig.1).
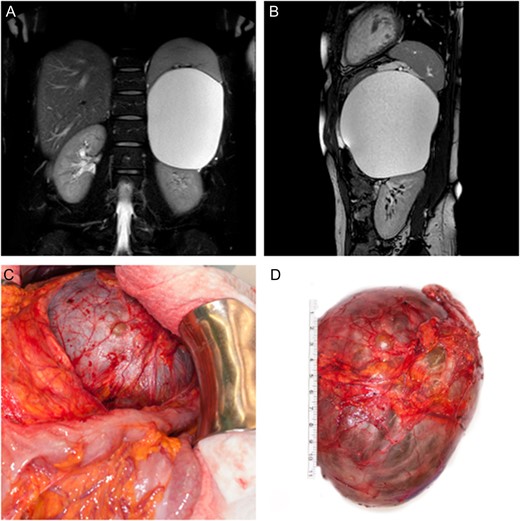
(A, B) Coronal and sagittal T2 weighted, fat suppressed MR image of the abdomen showing displacement of the spleen as well as the left kidney by the adrenal tumor. (C) Intra-operative finding showing close proximity of the cystic lesion to the left colonic flexure. (D) Surgically excised cystic tumor together with the left adrenal gland.
DISCUSSION
Among all of the reported cases, no single imaging modality was able to correctly diagnose an adrenal LA. Similar to our case, five adrenal LAs have even been characterized as a non-adrenal lesion prior to the operation [3]. A recent review of the literature concerning the general management of LAs concluded that treatment options should be individualized depending on size, symptoms and anatomic localization of the tumor [4]. With adrenal LAs being a very rare entity, the utilization of treatment guidelines for adrenal incidentalomas seems to be appropriate. If the cystic adrenal lesion is clinically and biologically inactive and its appearance remains unchanged over a period of 18 months time, conservative management is justified [5]. There is no evidence of reliable diagnostic value of preoperative biopsy or fine-needle aspiration for adrenal neoplasms [6].
Adrenal masses with either suspicious imaging aspects or size larger than 4 cm should be considered for resection due to a substantial risk of malignancy [7].
Up until now, only one adrenal LA has been resected using a retroperitoneoscopic approach and only three adrenal LAs have been treated via laparoscopic adrenalectomy [2, 3]. Taking in consideration that both the laparoscopic as well as retroperitoneoscopic approach result in reduced blood loss, less postoperative pain, shorter hospital stay and quicker recovery as compared to open surgery, minimally invasive surgery seems to be suitable for such lesions [8]. However, for adrenal neoplasms >10 cm in diameter, open adrenalectomy is recommended. This is due to the fact that these large adrenal masses may be diagnosed as malignant on definitive histologic analysis [9]. In our case laparoscopic adrenalectomy was not an option considering the enormous diameter of the cyst.
In histological examination, two cases of adrenal LA showed cellular atypia with a certain risk of malignant transformation [3, 10]. However, the available data regarding postoperative surveillance of adrenal LAs showed no signs of recurrence at 24-month follow-up after surgical resection. Therefore patients in whom the LA has been resected together with the adrenal gland are considered cured.
CONCLUSION
Up until today diagnosis of adrenal LAs cannot be established non-invasively. In order to diagnose and treat these lesions, adrenalectomy is considered the appropriate method for large (>4 cm in diameter) or symptomatic LAs. Small (<4 cm in diameter), clinically and biologically inactive adrenal cysts may be treated conservatively, provided that regular radiological surveillance can be warranted. Generally long-term follow-up showed excellent results and prognosis after resection of adrenal LAs.
CONFLICT OF INTEREST STATEMENT
The authors have no conflict of interest.
DISCLAIMER
The views expressed in the submitted article are not an official position of the institution or funder.



