-
PDF
- Split View
-
Views
-
Cite
Cite
Shane P Smith, Andrew F Feczko, Matias Mihura, Jey-Hsin Chen, Alexander S Farivar, Gastric hibernoma: a novel location and presentation of a rare tumor, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy105, https://doi.org/10.1093/jscr/rjy105
Close - Share Icon Share
Abstract
We present a case of gastric hibernoma, an unusual tumor with a location novel to the literature. A 39-year-old female presented with one year of upper gastrointestinal bleeding and dysphagia. Gastroenterology performed an esophagogastroduodenoscopy with ultrasound and identified a 6 cm mass within the muscularis propria of the antrum. Computed tomography demonstrated a 9.7 × 7.8 × 4.8 cm3 heterogeneous antral mass with internal septa. A distal gastrectomy with Bilroth I gastroduodenostomy was performed with 4 cm proximal and 2 cm distal margins. Excision was appropriate to make the diagnosis, exclude malignancy, and remove a symptomatic mass. Hibernoma was confirmed by histopathology. These are rare tumors of brown fat named for their resemblance to the thermogenic tissue found in hibernating animals. They typically present as a slowly enlarging mass of the thigh or shoulder. To our knowledge, this is the first presentation of a hibernoma as a submucosal gastric mass.
INTRODUCTION
Upper gastrointestinal (GI) bleeding is a common presentation requiring hospitalization; with ~100 per 100 000 hospitalizations annually in the USA [1]. The most common etiology of upper GI bleeds in the USA is ulcerative disease. GI neoplasia rarely presents as upper GI bleeding and even more uncommon are fat-derived gastric tumors [2]. Here, we present a rare cause of an upper GI bleed and a rare tumor with a location novel to the literature.
CASE REPORT
A 39-year-old female presented to her primary care physician with ~1 year of upper GI bleeding. She was a recent Ukrainian immigrant and had not undergone previous evaluation. She was referred to a gastroenterologist and underwent upper endoscopy with mucosal biopsy of a large antral mass. She declined endoscopic ultrasound (EUS) and was briefly lost to follow up over the course of a pregnancy. She returned to seek care for ongoing anemia and new epigastric pain. Esophagogastroduodenoscopy (EGD) with EUS was performed identifying a 6 cm mass within the muscularis propria of the antrum. Based on these findings, she was referred to a surgeon and underwent pre-operative computed tomography (CT) of the abdomen and pelvis which demonstrated a 9.7 × 7.8 × 4.8 cm3, heterogeneous mass with internal septa adherent to the posterior wall of the gastric antrum (Figs 1 and 2).
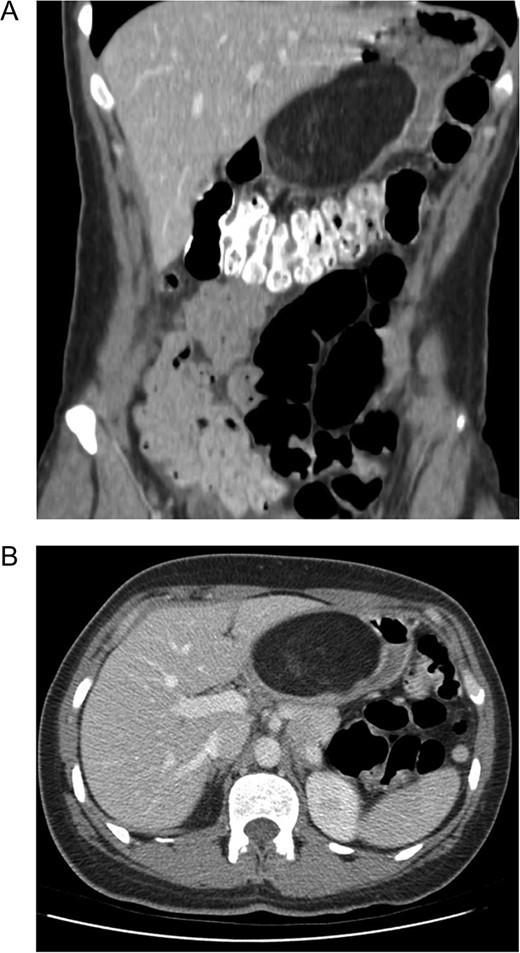
Computer tomography demonstrating a large (9.7 × 7.8 × 4.8 cm3) mural based mass extending along the posterior wall of the lesser curve of the stomach, effacing the lumen. (A) Coronal. (B) Axial. The mass contains predominantly fat signal with areas of hazy internal enhancement. No pathological lymphadenopathy was noted.
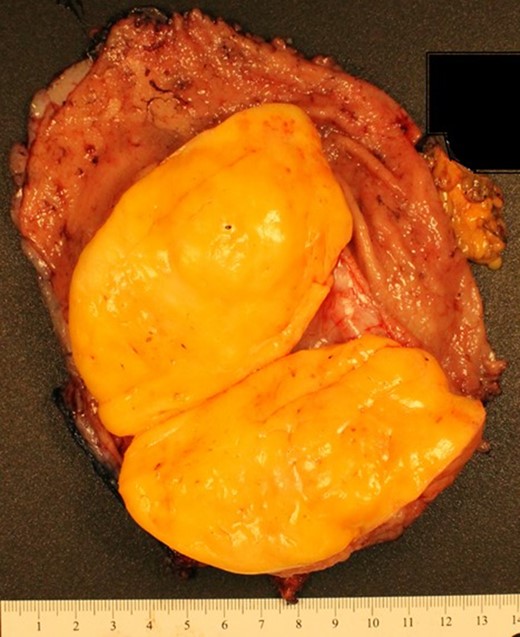
Gross pathology: partial gastrectomy specimen composed of distal portion of stomach and duodenum. Adipocytic neoplasm encapsulated and well circumscribed within the submucosa of the antrum. No gross or microscopic evidence of tumor necrosis. The tumor does not extend past the muscularis propria.
She was lost to follow up a second time before presenting to our emergency department with complaints of melena. Repeat EGD was notable for mucosal ulceration overlying the mass. Biopsy results were consistent with adipose tissue. With liposarcoma in the differential and the symptomatic nature of the mass, surgery was offered.
She ultimately underwent a laparoscopic exploration with plans for resection of this mass. This was converted to an open procedure due to the size of the mass and significant adhesion of the posterior gastric wall to the lesser sac. A distal gastrectomy was performed and 4 cm proximal and 2 cm distal margins were achieved. She was reconstructed with a Bilroth I gastroduodenostomy.
Her post-operative course was uneventful. Nutrition was provided enterally via a jejunostomy tube placed at the time of surgery and then advanced after a contrast study was completed without evidence of a leak. Following this she tolerated a general diet. She was discharged home on post-operative day eight.
Her final pathology was notable for a well circumscribed 10 × 7 × 5 cm3 yellow-orange mass within the wall of the antrum (Fig. 3). There was evidence of ulceration of the overlying mucosa, but no hemorrhage or necrosis within the mass itself. Histologically, the mass was composed of lipoma-like adipocytes (large, univacuolated cells with eccentric nuclei) intermixed with immature adipocytes (mutivacuolated cells with bland central nucleoli) and granular eosinophilic brown fat cells (Fig. 3). FISH MDM2 amplification testing was negative, ruling out well differentiated liposarcoma. Given this unusual histology and location, a second opinion was obtained and the unusual diagnosis of a hibernoma was confirmed.
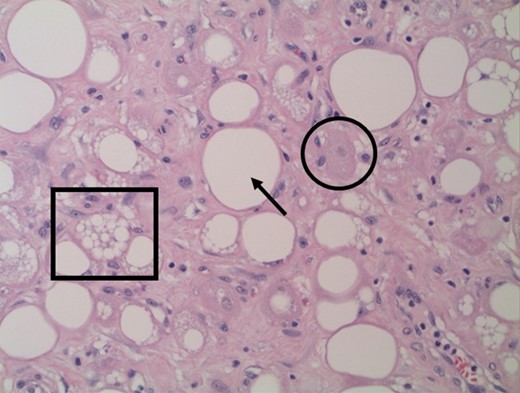
Histopathology of gastrectomy specimen (×200): Brown fat cells (circle) and scattered immature adipocytes (square) intermixed with Lipoma-like adipocytes (arrow), the later including. No mitotic figures or nuclear hyperchromasia identified.
DISCUSSION
Hibernomas are rare tumors of brown fat initially described by Merkel in 1906 for their resemblance to the thermogenic tissue found in hibernating animals [3]. In humans, brown fat is present in the fetus and newborn with the amount decreasing with age. It is widely distributed, with adult rests seen in the neck, axilla, mediastinum and inter-scapular regions [3–5]. Hibernomas are generally seen between the ages of 20–40 years [3–6]. They are believed to have a female predominance, although this has been called into question by the Armed Forces Pathology Institute study of hibernomas which showed a higher male occurrence (58%) [5]. Hibernomas are found throughout the body, most commonly in the thigh, shoulder, back and neck [5].
Hibernomas typically present as a slow growing palpable mass or with pain secondary to compression of surrounding structures. They are mobile and are found intramuscularly or subcutaneously [3–6]. CT imaging of these tumors demonstrates heterogenous, hypodense lesions. On T1 weighted MRI, hibernomas are hyperintense and similarly heterogenous. These findings, paired with the occasional intramuscular position of hibernomas requires histologic evaluation to rule out liposarcoma [3, 4]. Hibernomas are typically Flurodeoxyglucose (FDG) avid; consistent with their metabolic role in heat production, but PET scan cannot safely distinguish these tumors from malignant liposarcomas [6, 7]. On gross pathology, hibernomas are encapsulated and appear dark yellow to brown secondary to the higher number of mitochondria in these tumors [3, 4, 8]. Histologically, hibernomas are characterized by the presence of multi-vacuolated brown fat cells with eosinophilic cytoplasm and a small, central nucleus in the setting of normal adipose tissue (characterized by univaculated cells with an eccentric nucleus) [3, 5]. There are four histologic variants of hibernomas including typical (the most common), myxoid, lipoma-like and spindle cell, these are described separately but behave similarly [5].
To our knowledge, this is the first presentation of a hibernoma as a submucosal gastric mass. The differential for gastric mass is broad ranging from adenocarcinoma to GI stromal tumors to purely benign tumors like lipomas and leiomyomas. In this patient’s case, the presentation of GI bleeding was non-specific, but biopsy identifying lipomatous tissue narrowed the differential but did include liposarcoma. In this case, the diagnosis of hibernoma was not apparent by histology and therefore grossly negative margins were obtained as a precautionary measure. Hibernomas do not recur when completely excised and can usually be enucleated from the surrounding tissue [4, 5]. Excision was appropriate to confirm the diagnosis, exclude malignancy and remove a symptomatic rare tumor in an unusual location.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- ultrasonography
- computed tomography
- cancer
- deglutition disorders
- upper gastrointestinal endoscopy
- heterogeneity
- brown fat
- gastroenterology
- stomach neoplasms
- thigh
- diagnosis
- neoplasms
- shoulder region
- upper gastrointestinal bleeding
- hibernoma
- gastroduodenostomy
- billroth i procedure
- excision
- histopathology tests



