-
PDF
- Split View
-
Views
-
Cite
Cite
Suman Khanal, Yogendra P Singh, Rashmi Sharma, Rare case of bleeding nipple hemangioma in a lactating mother, Journal of Surgical Case Reports, Volume 2018, Issue 5, May 2018, rjy108, https://doi.org/10.1093/jscr/rjy108
Close - Share Icon Share
Abstract
Hemangiomas of nipple of the breast are rare lesions and are limited to case reports in the literature. Such pathology in a lactating mother are clearly a hindrance preventing the child from breastfeeding with its benefits. We report a rare case of a bleeding nipple hemangioma in a 24 years old lactating mother with the clinical, imaging and histopathological findings.
INTRODUCTION
The increasing awareness regarding the breast cancer has led the nipple growths to be alarming to the patient. It is therefore important for breast surgeons to be able to correctly diagnose these lesions. Hemangiomas of breast are rare benign vascular lesions without endothelial hyperplasia, atypia and inter-anastomosing vascular channels of angiosarcoma [1, 2]. They can occur in any age group. Though there are no epidemiological data on prevalence of benign tumors of nipple, a case series by Spyropoulou et al. [3] included four benign lesions of nipple. However, none were hemangioma. In this report we present a rare case of bleeding nipple hemangioma in a lactating mother and review the literature.
CASE REPORT
A 24-year-old lactating mother from Dhading district of Nepal presented with a bluish discolored swelling in her left nipple for 2 months. The swelling was initially small in size present on the superior aspect of left nipple that grew to a current size over a course of month. She has a 10 months old child and was having difficulty breastfeeding from left breast.
Before current presentation in our Breast and Thyroid Unit, she had presented in emergency for bleeding from the swelling 5 days back which was managed with compression bandaging.
The patient came to our Unit for further management. The patient does not have any co-morbidities including liver disease.
She is a non-smoker, consumes alcohol occasionally. She does not have history of malena, hematemesis, epistaxis, hormonal contraceptive use or radiotherapy. She had menarche at the age of 16 years and works as homemaker.
The patient is fairly built with no anemia or bruises over the body. There was a 2 × 1.5 cm swelling in the superior aspect of left nipple with bluish discoloration of the surface. There was a scab medially, the site of bleeding for which patient had presented earlier in emergency. The swelling was partially compressible. On retro-areolar application of gentle pressure, there was milk discharge from the ducts below the swelling. The patient did not have axillary lymphadenopathy and signs of chronic liver disease.
The patient had normal complete blood count and coagulation profile. Renal function was normal. Patient was seronegative for HIV, HBV and HCV.
Ultrasound of the swelling revealed 2 × 1.5 cm well defined heteroechoic lesion with marked vascularity with both arterial and venous patterns of waveform in superior aspect of left nipple. Rest of the breast, areola and axilla were normal.
The diagnosis of vascular lesion was made. Given the risks of re-bleeding and difficulty in breastfeeding, we decided for excision of the lesion after discussion of the risks of surgery (possibility of need of excision of nipple should the need arise and consequent affection of breastfeeding). Excision was uneventful.
The resected specimen was firm, well circumscribed mass with cystic spaces.
Histopathological examination of the lesion showed keratinized stratified squamous epithelium with underlying stroma showing proliferation of capillary blood vessels separated by fibrous connective tissue. The capillaries were lined by bland epithelial cells. Thus, the diagnosis of capillary hemangioma of nipple was made (Figs 1–5).

Photograph showing the lesion on superior aspect of left nipple.



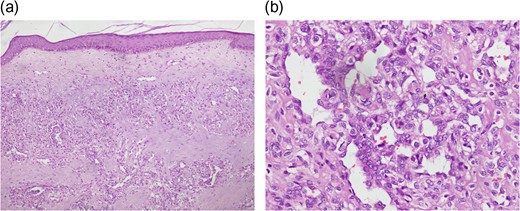
Histopathology showing stratified squamous epithelial lining with proliferation of capillaries in underlying stroma (H & E stain). (a) 10× Magnification (b) 40× Magnification.
At 3 months follow up, patient was doing fine and was breastfeeding.
DISCUSSION
Though common in other parts of body, there are few reported examples of hemangiomas of breast. More so are the capillary hemangiomas of nipple. In the 16 cases of breast hemangiomas studied by Mesurolle et al., 14 were cavernous and only 2 were capillary hemangiomas [4]. There is only a single case of bleeding hemangioma of nipple in literature in a 16 years old male [5]. Though cavernous hemangiomas of breast are more likely to present as bleeding, our case is unique in that it was a capillary hemangioma. It can be argued that bleeding could have been due to trauma of breastfeeding, but it could not be only one factor. The rapid increase in size during lactation and the increased vascularity during lactation are other factors. Though florid papillomatosis are the common lesions to present with bleeding from nipple, a high index of suspicion for the possibility of hemangioma should be kept in mind [5]. Complete excision is recommended for all hemangiomas of breast including nipple to exclude the possibility of underlying low grade angiosarcoma [6] and due to the difficulty of correct preoperative diagnosis [7, 8]. The diagnosis of benign vascular tumors of the breast should be achievable based on microscopic findings alone in most cases. Only in doubt the specimen can be evaluated for expression of endothelial cell markers (CD31, CD34, factor VIII and Fli-1) [9] which was not required in our case.
CONCLUSION
Though rare, hemangiomas of breast and especially the nipple can have a significant esthetic and functional concern, and can increase in size during lactation. Capillary hemangioma should also be considered in bleeding nipple lesions if it grows relatively rapidly during lactation. Excision is advised to rule out the possibility of low grade angiosarcoma, facilitate breastfeeding and reduce anxiety.
ACKNOWLEDGEMENTS
Dr Anuja Bhandari, Resident, Department of Pathology.
CONFLICT OF INTEREST STATEMENT
None of the authors has any conflict of interest to report.
FUNDING
No funding was received from any source for this work.
CONSENT
Written informed consent was obtained for publication of this report and accompanying images.



