-
PDF
- Split View
-
Views
-
Cite
Cite
Jose’ F Velasquez, Gisella Nele, Salvatore Giordano, Abdominal tattoo can be useful to avoid a midline abdominal incision, Journal of Surgical Case Reports, Volume 2018, Issue 4, April 2018, rjy071, https://doi.org/10.1093/jscr/rjy071
Close - Share Icon Share
Abstract
We report a case in which abdominal tattoo margins were modified and used to hide the surgical incision for desmoid tumour removal. Our patient is a 37-year-old female with history remarkable for atrial septal defect closure at the age of ten, but not for previous abdominal surgeries or trauma. A desmoid tumour diagnosis was made upon needle biopsy of the 5 × 4 cm2 mass confined to the rectus abdominis. Subsequently, tumour was resected with an incision through the tattoo upper margin and abdominal wall was reconstructed with primary fascial closure mesh reinforced. Excision was radical, scar inconspicuous and no incisional hernia, bulging, nor tumour recurrence were detected at 2-year follow-up. This report highlights the fact that an abdominal tattoo might be considered as incision access instead of typical midline incision.
INTRODUCTION
The practice of body tattooing has increased considerably in the last decade. In 2012, a US national data survey revealed that body tattoo was prevalent in 18% of adult male between 18 and 49 years and 16% in 50 and 69 years, and female 29 and 7% respectively. Particularly, the lower back, the shoulder and the ankles are the favourite locations in women, while in men it is most common to find tattoos on the torso and arm [1, 2]. In plastic surgery settings, skin tattoos can be considered a problem because the images can be located within the operative field interfering with the standard placement of surgical incisions; they can also interfere with the scaring process due to granulomatous reaction on some components of the inks used, or they even can hide dermatologic pathologies such as melanomas that might modify the prognosis for eventual further surgical procedures [3, 4]. The cost of the tattoo might be relatively high (up to 1400 usd) and can be considered a remarkable aspect of the person identity, therefore, it is extremely important to considerate its preservation during surgery [2–5]. Here, we report a case in which tattoo margins were used as surgical incision access for the removal of a desmoid tumour with patient’s consent.
CASE REPORT
A 37-year-old female, otherwise healthy patient, presented to observation with a 3-month history of a mass in the upper right side of the abdomen, which has been gradually increasing in size, and no other associated symptoms. Past medical history was remarkable for atrial septal defect closure at the age of ten, but no previous abdominal surgeries or trauma. Patient did not smoke, drink alcohol or took any medication. During the physical examination, inspection showed a tattoo on the right side of the umbilicus (Fig. 1A); palpation at the same level revealed a painless and firm mass of 5 × 4 cm2 approximately, with not easily definable edges. Ultrasonography showed a 4 cm2 mass with no clear margins. Abdominal magnetic resonance (MRI) was subsequently performed describing a 17 × 19 × 50 mm3 mass confined into the rectus abdominis (Fig. 2A and B). Needle biopsy samples were taken, and pathology report confirmed the diagnosis of a desmoid tumour.
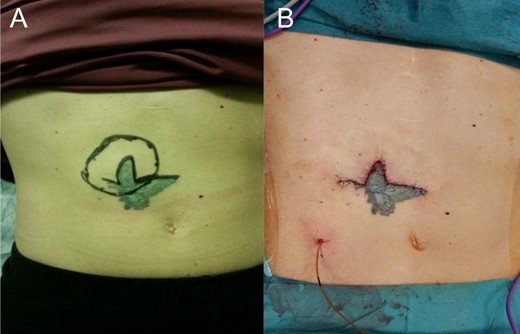
(A) The abdominal tattoo before the operation and the tumour is beneath it. (B) Surgical scar along the margin of the tattoo.
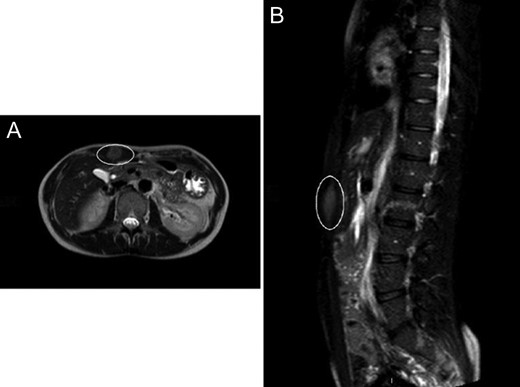
(A) Abdominal CT showing the desmoid tumour within the abdominal wall. (B) Abdominal CT scan showing lateral view of the desmoid tumour.
The surgery for the mass removal was performed under general anaesthesia and the incision was placed in the upper edge of the tattoo, just above the tumour localization (Fig. 1). A segment of 7 × 5 × 3 cm3 was resected from the rectus abdominis. Abdominal wall was subsequently reconstructed with primary fascial closure reinforced with underlay polypropylene mesh. Local bupivacaine infusion catheter was placed for pain control [6]. Abdominal suture was carried out in three layers abdominal fascia using Vicryl 3-0 for abdominal fascia and dermis, and skin with single stiches prolene 4-0 (Fig. 1B). Wound healing was uneventful and the specimen confirmed a desmoid tumour, without mitotic or necrotic features, radically excised. At three months follow-up the scar was difficult to notice because of the tattoo. At 2-year follow-up, the patient was satisfied with his tattoo scar, while no tumour recurrence revealed by MRI, either abdominal hernia nor bulging could be detectable (Fig. 3B).

DISCUSSION
Although skin tattoos are still considered taboo in the western society, this ancient art form is gaining more followers every day. This prehistoric art manifestation goes back almost 2000 years ago when the first Polynesian societies used to wear them to symbolize bravery, leadership, power or the representation of a reached milestone within the community [7]. Nowadays, tattoos are considered a way to communicate individuality and freedom as well as cosmetic body improvement [2, 7]. Some tattoo techniques have been implemented in the medical field ranging from identifying non-palpable tumours in neck and breast, camouflage various scars for cosmetic improvement or nipple reconstruction after mastectomies, body identification assistant for forensics, field marking radiation in oncology or as a warning for chronic disease or life threatening allergy [3, 8, 9]. According to recent data, 79% of surgeons had encountered tattoos at proposed incision sites and 61% preferred to relocate the incision site to avoid patients complaint for tattoo disruption [5]. Although little is written on how to proceed in case of tattoo in the surgical field, literature mostly converges to plan the surgery in advance including and respecting patient will. Different strategies have been described to preserve a tattoo according to its dimensions and location: small tattoos represent no limitations for surgical wound placement while medium size and large coloured tattoos can be preserved either by making the incision at the margin of the tattoo or inside the tattooed area [10]. In our case, the tattoo was almost on the tumour side and permitted to avoid a midline abdominal incision (Fig. 1A and B). The interface between the upper edge of the tattoo and the skin was used to camouflage the surgical incision (Fig. 3).
Whenever tattoos are present in the surgical field, we recommend to consider them as a possible incision access, not only in order to preserve the tattoo, but also for an invisible scarring. In this way, the tattoo itself can be used to camouflage the incisions and subsequent scars allowing a better aesthetic result, concealing patient’s and surgeon’s satisfaction.
CONFLICT OF INTEREST STATEMENT
The authors have no financial interest to declare in relation to the content of this article.



