-
PDF
- Split View
-
Views
-
Cite
Cite
Andrew Tan, Ran Li, Mohammed Rafique, Sharon Qin, Toan Pham, A rare case of giant extra-ovarian mucinous cystadenoma arising from sigmoid mesocolon, Journal of Surgical Case Reports, Volume 2018, Issue 3, March 2018, rjy038, https://doi.org/10.1093/jscr/rjy038
Close - Share Icon Share
Abstract
An 80-year-old female presented with one month history of acutely worsening abdominal distention and pain, without features of bowel obstruction. A giant intra-abdominal simple cyst, separate from the ovaries, was seen on imaging. Initial haematological and biochemical investigations, including tumour markers, were normal. At laparotomy, the cystic tumour was discovered to arise from the sigmoid mesocolon and was resected en bloc. Histopathology revealed the tumour to be a benign extra-ovarian mucinous cystadenoma, which is a neoplasm of ovarian origin that can arise from extra-ovarian sites, including the mesentery. Extra-ovarian mucinous cystadenoma arising specifically from the mesentery are very rare intra-abdominal neoplasms with malignant potential despite its benign appearance on investigations. This case aims to raise awareness of this condition and to highlight its diagnostic approach and surgical management.
INTRODUCTION
Mucinous cystic neoplasm (MCN) are surface epithelial tumours of ovarian origin that can arise from extra-ovarian sites including pancreas, appendix, hepatobiliary tract and rarely the mesentery and retroperitoneum [1–4]. Generally, the vast majority of ovarian MCNs are benign or histologically borderline tumours. They typically occur in mid adult life [3] and are rare before puberty or after menopause [5]. The most common subtype of MCN is mucinous cystadenoma, which is typically large, multi-loculated and filled with gelatinous fluid rich in glycoproteins [5, 6]. The cyst wall of extra-ovarian MCNs is encapsulated by a fibrous capsule, lined by mucin-secreting epithelium and goblet cells, and associated with an underlying sub-epithelial ovarian like stroma (OLS) [1, 6]. The OLS stains strongly for alpha-smooth muscle actin (alpha-SMA) and vimentin and weakly for desmin. Both oestrogen and progesterone receptors are expressed in the nuclei of OLS cells [4].
Cases of mucinous cystadenoma arising specifically from the mesentery are rare with only 17 cases previously reported in the literature [3]. There are no known risk factors aside from age (mean = 32 ± 13) and gender (predominantly female) [3]. The pathogenesis of extra-ovarian MCNs remains incompletely understood, and is further confounded by their discovery in two men [3]. Some of the more widely accepted theories that have been proposed include mucinous metaplasia in pre-existing mesothelial cysts, invaginated peritoneum along the course of ovarian descent, coelomic metaplasia of epithelial cells and neoplastic differentiation of epithelial cells from a secondary extragenital Mullerian system [1, 7–10].
Unlike its ovarian counterpart, extra-ovarian mucinous cystadenoma arising from the mesentery has malignant potential with 42% identified as such in 17 cases [3].
We present a case report of a giant benign extra-ovarian mucinous cystadenoma arising from the sigmoid mesocolon.
CASE REPORT
An 80-year-old female presented to our health service with one month history of acutely worsening abdominal distention and pain, on a background of six months of non-specific gastrointestinal symptoms which was investigated with an abdominal ultrasound that did not detect any abnormality. Relevant medical history includes vaginal hysterectomy secondary to fibroids, type 2 diabetes mellitus, hypothyroidism, hypercholesterolaemia and hypertension.
On history, the main symptoms were abdominal distention and pain with no features of bowel obstruction. The vital signs were within normal limits. On examination, the abdomen was grossly distended with focal tenderness in the upper abdomen. There was a palpable cystic mass which appears of pelvic origin, however, the gynaecological examination was normal.
Routine laboratory investigations were normal. Tumour markers, including CA 125, CA 15-3, CA 19-9 and CEA, were all within normal limits.
A contrast-enhanced CT scan of the abdomen and pelvis was performed, which revealed a large intra-peritoneal cyst measuring 21 × 25 × 26 cm3, containing simple fluid (Fig. 1). There were a few thin septations along the periphery with no appreciable nodular or soft tissue components within. The origin of the cyst was not able to be determined due to gross displacement of surrounding viscera. There was associated splaying of the bowel loops without resultant bowel obstruction. No pathologically enlarged abdominal, pelvic or inguinal lymph nodes were noted and there was no vascular compromise. On pelvic ultrasound, the majority of the lesion appeared simple cystic in nature. There was no obvious internal colour flow. Both ovaries were identified and appeared separate from the cyst.
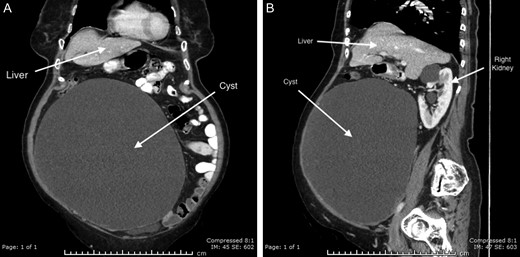
CT abdomen with IV and oral contrast; (A) coronal and (B) sagittal.
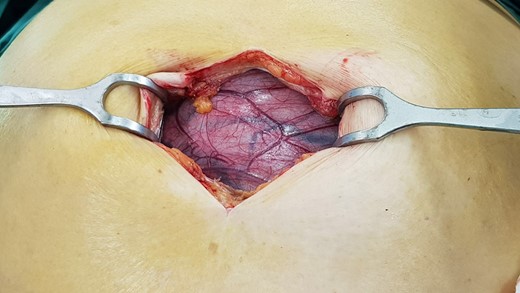
A laparotomy was performed to resect the cyst for diagnostic and therapeutic purposes (Figs 2 and 3). The cyst was noted to originate from the sigmoid mesocolon. No other viscera required resection. The patient made an uneventful recovery.
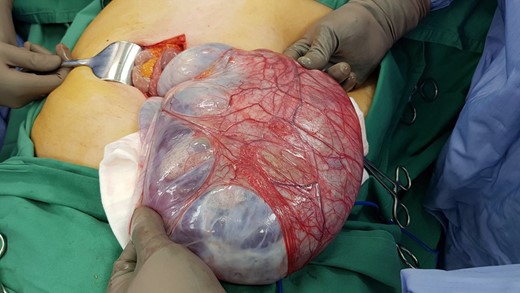
Macroscopically, there was an intact cystic structure containing clear yellowish serous fluid. The internal surface was smooth with wall thickness of up to 10 mm. On microscopy, the cyst was lined by a single layer of columnar cells with apical mucin and had surrounding ovarian stroma. There was no evidence of malignancy. The cystic tumour was confirmed to be a benign mucinous cystadenoma of the ovary arising from the sigmoid mesocolon.
DISCUSSION
Cases of extra-ovarian mucinous cystadenoma arising from the mesentery are very rare. Due to its rarity and typical benign appearance as a simple cyst, extra-ovarian mucinous cystadenoma is a diagnostic challenge to clinicians and may not be pre-operatively recognized as a neoplasm with malignant potential. Through our case presentation, we offer a diagnostic and surgical approach to its management.
Imaging provides the pre-operative differential for extra-ovarian MCNs. On CT, the tumour is typically a well-circumscribed, uni-loculated cystic lesion containing simple fluid which does not enhance with contrast. Occasionally, internal septations or peripheral calcification of the capsule can be seen [3]. As MCNs can be large, CT is able to assess for anatomical relationship between the tumour and surrounding structures [11]. On ultrasound, MCNs share similar features as a simple cyst: well-defined, uni-loculated cyst containing slightly echoic fluid. Pelvic ultrasound may also be used to determine whether the MCN arises from the ovary.
Haematological and biochemistry investigations are often unremarkable. Tumour markers such as CA 19-9 may be elevated in ovarian and pancreatic MCNs but not in those arising from the mesentery [3]. Therefore, there is no clear evidence on the diagnostic utility of pre-operative tumour marker.
Pre-operative aspiration of the cystic fluid for cytological analysis is not recommended for two reasons. In the 17 cases of extra-ovarian mucinous cystadenoma arising from the mesentery, malignancy (high grade dysplasia and cystadenocarcinoma) was demonstrated in eight cases (42%) [3]. Spillage of potentially malignant mucin into the peritoneum may cause seeding of malignant cells and development of Pseudomyxoma peritonei. Additionally, cytological analysis of the aspirated fluid provides little diagnostic value as it frequently fails to reveal the type of epithelial cells lining the cyst [12]. Therefore, and for similar reasons, we do not recommend intraoperative decompression of the cyst via aspiration. Given the significant risk of malignancy, en bloc resection of mesenteric MCNs is recommended for suitable surgical candidates.
ACKNOWLEDGEMENTS
The authors are thankful to the patient who had provided written informed consent.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interest regarding the publication of this article.



