-
PDF
- Split View
-
Views
-
Cite
Cite
Steve I Lindley, Paul M Peyser, Idiopathic omental infarction: One for conservative or surgical management?, Journal of Surgical Case Reports, Volume 2018, Issue 3, March 2018, rjx095, https://doi.org/10.1093/jscr/rjx095
Close - Share Icon Share
Abstract
Idiopathic omental infarction (IOI) is a rare cause of right-sided abdominal pain, mimicking serious surgical pathology. It occurs in <4 in 1000 cases of appendicitis. IOI can be a challenge to diagnose, as features may mimic appendicitis, and therefore in young patients, may only be discovered on laparoscopy. CT features can be diagnostic, but due to its rarity the diagnosis may be unclear. The literature supports both conservative management and surgical management (to expedite symptom resolution). We present a case of IOI and discuss our management and learning from the case. We discuss the utility of CT radiology, conservative management and the benefits of non-resection management, even at laparoscopy.
INTRODUCTION
Idiopathic omental infarction (IOI) is a rare cause of right-sided abdominal pain, which can mimic the common presentations of both acute appendicitis and acute cholecystitis [1]. Since improvements to CT imaging and availability of laparoscopy, increasing reports of IOI has triggered a debate about how it is best managed. We present a case of IOI and discuss its management.
CASE REPORT
A 42-year-old man presented to the surgical take via the emergency department with severe right-sided abdominal pain. The patient had no significant medical or surgical history. His BMI was 29. He reported a first episode of sudden onset worsening non-colicky abdominal pain over his right iliac fossa extending to his right upper quadrant. He remained hungry and did not experience any gastrointestinal symptoms.
The gentleman’s observations were within normal limits and his initial temperature was 37.0°C. He was tender over the right side of his abdomen, without peritonism. Murphy’s sign was elicited. His examination was otherwise unremarkable. Urinalysis was normal. Blood tests revealed an elevated white cell count (10.9 × 109/L) and C-reactive protein of 98 mg/L. All other blood tests were normal.
An initial differential diagnosis was made as cholecystitis. Appropriate intravenous antibiotics were commenced. An abdominal ultrasound demonstrated a thin-walled gallbladder without gallstones and a normal common bile duct caliber. There was however a trace of free fluid in the right iliac fossa. The sonographer was unable to identify a normal appendix. The following afternoon a CT scan of his abdomen and pelvis demonstrated fluid in the right iliac fossa as well as his rectovesicular pouch. The appendix was normal, but there was tissue stranding adjacent to the caecum and ascending colon to the tip of the liver (Figs 1 and 2).
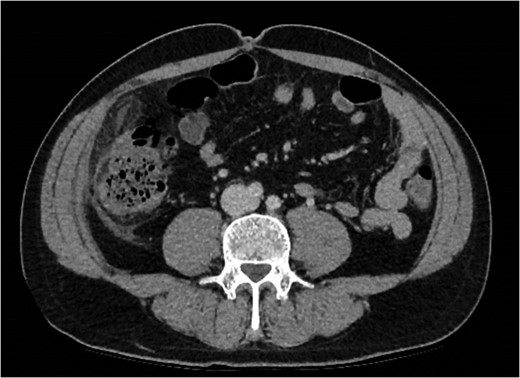
Abdominal CT demonstrating soft tissue stranding anterio-lateral to the ascending colon/caecum without evidence of bowel wall thickening.

Abdominal CT demonstrating soft tissue stranding and odema inferior to a normal gallbladder, extending to the caecum.
This gentleman was initially managed conservatively, with a low threshold to perform a diagnostic laparoscopy should his symptoms worsen.
Later that evening, he amounted a pyrexia of 37.8°C, he did not feel he was improving, and he was still tender. Diagnostic laparoscopy was arranged with a view to ensuring he was not developing appendicitis.
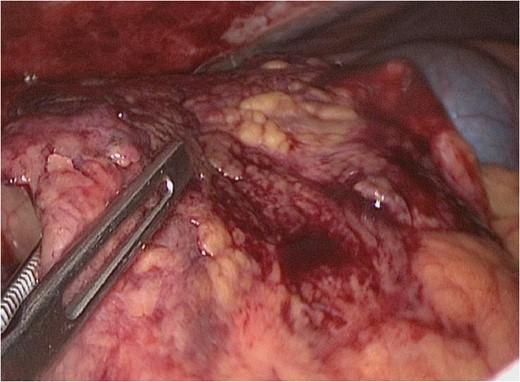
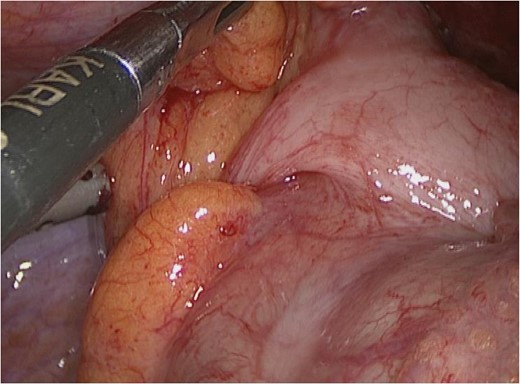
On laparoscopy, a 7–10 cm right-sided segment of greater omentum was inflamed and necrotic, without adjacent mischief or signs of omental torsion (Fig. 3). The caecum and ascending colon were entirely normal (Fig. 4). The appendix was retrocaecal and retroperitoneal. The appendix was not dissected to visualize the entire length; the infarcted omentum was discrete to this. An omental necrosectomy was not performed due to the risks of this bleeding and potential diathermy injury risk. Rather, accepting the risk of protracted symptoms from minor omentum necrosis.
The patient felt much better postoperatively. On further questioning he denied a family history of thrombophilia. A thrombophilia screen was unremarkable. He was discharged 36 h later. Telephone follow-up revealed that he only required paracetamol for 8 further days to control ‘discomfort’.
DISCUSSION
IOI is a rare cause of right-sided abdominal pain, which can mimic both appendicitis and acute cholecystits in a ratio of 2/3 to 1/3 [1, 2]. Reports suggest an incidence of <4 in 1000 cases of acute appendicitis [3]. Previous cases highlight the preponderance for right segmental infarction, owing to tenuous vasculature in this region, and relating to right-sided symptomatology [5]. Obesity is a known risk factor; the hypothesis being that a fatty omentum may occlude its own distal atrial branches [4]. Conversely, there are reports of cases in healthy marathon runners citing that low omental blood flow and physiological shunting, risks infarction [5].
Decision to laparoscope
This case was consistent with other presentations of IOI. Ultrasound reassured against cholecystitis and CT findings made appendicitis unlikely, however, the reporter did not commit to a radiological diagnosis. Retrospective radiological diagnoses include IOI and epiploic appendagitis. The latter being unlikely as inflammation is normally limited to <5cm. Taking into account the specificity of CT for appendicitis, a stronger case for conservative management could have been raised. However, CT sensitivity for IOI is reported as 90% [6]. In light of an unclear radiological diagnosis but evidence of abnormality (free peritoneal fluid in a man), a new fever and ongoing pain, a laparoscopy was justified.
Omental necrosectomy vs non-resection management
Without necrosectomy, pain can persist for an average of 13.5 days [2]. Omental necrosectomy reduces the duration of abdominal pain, speeding up a patients’ discharge and return to normal activity [7]. However, there are only scarce reports of omental abscess formation following conservative treatment [8].
The use of electrosurgical dissection equipment is associated with a potentially life-threatening risk of unrecognized thermal injury of 1–5/1000 cases [9, 10]. This risk is reduced with expensive intelligent ultrasonic/electrosurgical equipment [11]. In light of this small risk, and only a small area of necrosis, we perceived the risk to be greater with resection. Our patient was discharged within 36 h postoperatively, only requiring simple analgesia on discharge and was pain-free after 9 postoperative days. These features represent only minor postoperative morbidity and justify our non-resection approach.
CONCLUSION
IOI is a benign condition, which can mimic, both clinically and radiologically, serious intra-abdominal pathology. While patients with this diagnosis can avoid an operation, concerns over more serious pathology may trigger laparoscopy.
Attempts should be made to reassure against serious pathology and diagnose IOI with appropriate imaging. CT has been shown to be sensitive, but may require an experienced GI radiologist to reassure further.
Despite previous cases supporting necrosectomy, justified only by expediting symptom resolution, our non-resection management was only associated with the requirement of simple analgesia for 9 days. This was acceptable to the patient.
In summary, consider the diagnosis of intra-abdominal fat necrosis (IOI and epiploic appendagitis) in presentations of right-sided abdominal pain without GI symptoms, and consider conservative management, providing serious pathology is reasonably excluded.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



