-
PDF
- Split View
-
Views
-
Cite
Cite
Eoghan Burke, Tara Connelly, Abeera Mehmood, Maurice Murphy, Gerrard O’Donoghue, Brown bowel syndrome, an unusual cause of sigmoid volvulus, Journal of Surgical Case Reports, Volume 2018, Issue 3, March 2018, rjy039, https://doi.org/10.1093/jscr/rjy039
Close - Share Icon Share
Abstract
We report a case of a 79-year-old gentleman who presented to the emergency department with a 5-day history of abdominal pain, constipation, a progressively distending abdomen and new onset feculent vomiting on a background of a recent endoscopic decompression of a sigmoid volvulus. Investigations confirmed the presence of a recurrent sigmoid volvulus. Attempts to reduce this endoscopically failed and laparotomy with sub-total colectomy and ileostomy formation was performed. Histology from the resected specimen identified a distinct pathology, namely intestinal lipofuscinosis also known as brown bowel syndrome. Brown bowel syndrome is a recognized but rare complication of chronic long term malnutrition. It may present in a myriad of ways including atonia and, rarely, massive colonic dilatation, as in our case.
INTRODUCTION
Intestinal lipofuscinosis, also known as brown bowel syndrome, is characterized by a pathological accumulation of cytotoxic lipofuscin within smooth muscle cells of the muscularis propria. It is most commonly seen in chronically malnourished older patients. A major risk factor is Vitamin E deficiency evidenced by the fact that vitamin E supplementation can correct the pathology if identified early enough [1].
CASE REPORT
A frail 79-year-old gentleman, Mr X, presented to the emergency department (ED) complaining of a five day history of abdominal pain and constipation associated with progressive abdominal distention and one day history of feculent vomiting.
His past medical/surgical history was significant for an open cholecystectomy performed 20 years ago, umbilical hernia repair over 50 years ago, type 2 diabetes mellitus, COPD and a recent admission (2 months previously) with a sigmoid volvulus which was decompressed at endoscopy.
He was not prescribed any regular medication and was allergic to penicillin and paracetamol.
His family history was non-contributory.
Mr X reported a history of excessive alcohol intake, 16–20 units per week, and was an ex-smoker of 20 years.
Vitals in ED were all within normal limits.
On examination Mr. X was comfortable at rest. His abdomen was distended and tympanic but non-tender and bowel sounds were normal. There was a large reducible peri-umbilical hernia.
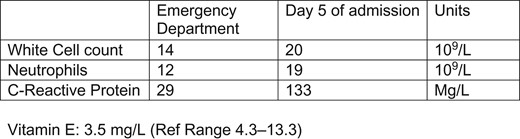
Bloods are illustrated in Fig. 1.
Mr. X had a plain film abdominal x-ray taken in ED which displayed dilated loops of bowel, Fig. 2. CT abdomen and pelvis was performed which showed an abrupt transition point in the sigmoid colon and a twisting of the sigmoid colon consistent with a volvulus, Fig. 3.

Plain film abdominal X-ray taken on admission. Note coffee bean sign in Left iliac fossa.

CT abdomen/pelvis. Note large umbilical hernia with loops of bowel within. Note abrupt transition point at centre of Image.
In light of these findings, Mr. X was admitted to the surgical ward and kept nill-per-oral with naso-gastric tube in situ.
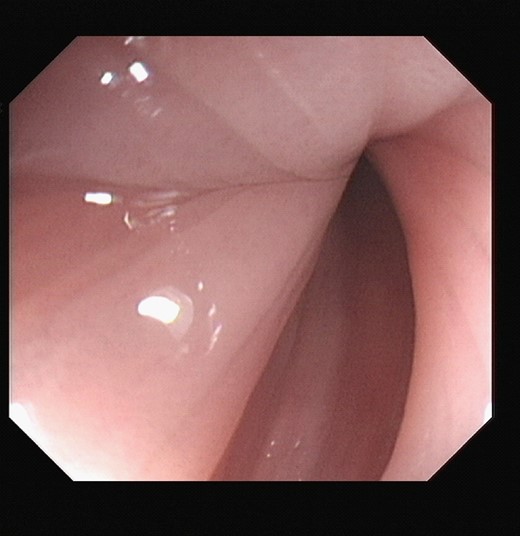
At sigmoidoscopy, the volvulus was successfully decompressed. The mucosal lining was pink and healthy in appearance, Fig. 4. Mr. X improved following this intervention.
Unfortunately on the fifth day of Mr. X’s admission, he became acutely unwell with left iliac fossa pain and vomiting. Repeat sigmoidoscopy revealed a blue mucosa which appeared ischaemic with no visible peristalsis. Attempted decompression was unsuccessful, Fig. 5.
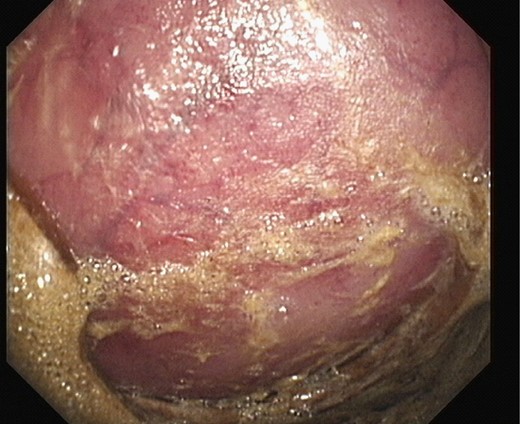
Repeat sigmoidoscopy: bluish discolouration of mucosa concerning for ischaemia.
Mr. X underwent a sub-total colectomy and ileostomy formation secondary to ischaemic sigmoid volvulus and a diffusely dilated colon.
The resected portion of sigmoid colon measured 18 cm in circumference. The muscularis propria showed increased amounts of intracellular lipofuscin, which was perle’s stain negative, and both PAS and PAS/D positive, Fig. 6.
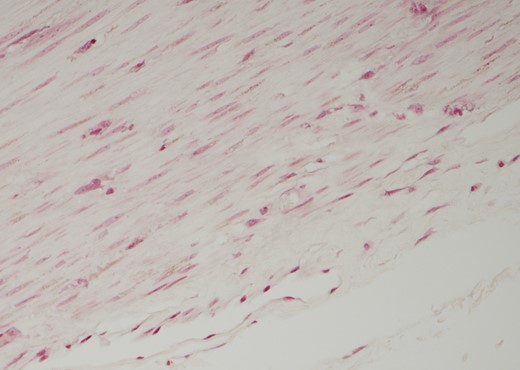
Histology: section of muscularis propria. Staining positive for both PAS and PAS D. Perle’s stain was negative.
These findings supported a diagnosis of intestinal lipofuscinosis.
DISCUSSION
Intestinal lipofuscinosis, or brown bowel syndrome, is a pathology characterised by the pathological deposition of lipofuscin predominantly within the smooth muscle cells of the muscularis propria [2].
Lipofuscin consists of oxidized proteins, and to a lesser degree oxidized lipids [3], which act as potent free radicals intracellularly.
Lipofuscin exists physiologically in certain tissues and its concentration increases as we age [4]. Lipofuscin accumulates in the setting of increased oxidative stress and reduced anti-oxidizing ability of the aging host cell [5].
Brown bowel syndrome occurs when lipofuscin accumulates to pathological levels in the muscularis propria [6]. When an added insult, most commonly malnutrition, is superimposed on an aging system, intestinal lipofuscinosis is more common. This is largely believed to be due to a deficiency of vitamin E [7], which is a potent anti-oxidant [8]. Thus older malnourished patients are at increased risk of developing intestinal lipofuscinosis.
The oxidative stress results in necrosis and autophagy of smooth muscle myocytes of the muscularis propria [9]. This can present as atonia or rarely massively dilated bowel as occurred in our case.
CONCLUSION
In conclusion, intestinal lipofuscinosis, also known as brown bowel syndrome, is a condition characterised by a pathological accumulation of cytotoxic lipofuscin within smooth muscle cells of the muscularis propria [10]. It presents clinically in a multitude of ways including massive dilatation of the atonic bowel, as in our case.
This case presents an uncommon cause of sigmoid volvulus and highlights the importance of adequate nutrition in older patients whose physiological anti-oxidant pathways are already compromised.
CONFLICT OF INTEREST STATEMENT
None declared.



