-
PDF
- Split View
-
Views
-
Cite
Cite
Raashad Hasan, Wiqqas Jamil, Case report of a ruptured endobutton used in medial patellofemoral ligament reconstruction causing patellofemoral impingement, Journal of Surgical Case Reports, Volume 2018, Issue 2, February 2018, rjy025, https://doi.org/10.1093/jscr/rjy025
Close - Share Icon Share
Abstract
The medial patellofemoral ligament (MPFL) is a key soft tissue stabilizer of the medial patella, with deficiency proven to be a key contributor to patellar dislocation. Reconstruction of this ligament has become a widely employed procedure in managing patients with recurrent patellar dislocation, and is also gaining popularity in the setting of primary dislocation. A wide variety of techniques have been described, differing in the type of graft used, sites for fixation and fixation technique. A number of complications have also been reported in the literature, including post-operative stiffness, apprehension, patellar fracture and recurrence of instability and dislocation. Here we report a case of an endobutton used in MPFL reconstruction becoming displaced after minimal trauma in a young female patient, subsequently causing patellofemoral irritation, patellar cartilaginous damage and functional limitation. This complication has not been previously reported to our knowledge and is one that surgeons must be aware of.
INTRODUCTION
The medial patellofemoral ligament (MPFL) acts as the primary medial stabilizer of the patella between full extension and 20° of flexion [1]. Due to this role, incompetence of the MPFL has been widely accepted as a major factor in patellar dislocations. Open macroscopic examination of 67 knees with either acute or chronic patellar dislocation found abnormalities in all cases, varying from loose attachment and scar tissue formation to total absence and rupture [2]. These findings have also been correlated via MR imaging [3]. Thus, reconstruction of this ligament has become a popular technique in managing patients with patellar dislocations.
A variety of techniques have been described in MPFL reconstruction. Similarly, a variety of post-operative complications have also been reported. Here, we report a unique case of an endobutton used for anterior femoral cortex graft fixation becoming traumatically displaced following minimal trauma. We conclude that this complication was due to erroneous initial tunnelling technique, and make suggestions how to avoid such a complication if tunnelling goes awry.
CASE PRESENTATION
A 19-year-old female presented to fracture clinic 1 day after sustaining a twisting injury to her right knee. At presentation the knee was mildly swollen without effusion. There was significant tenderness on the medial patella. A longitudinal medial para patellar scar and longitudinal medial scar over the MCL were noted. Range of motion was 0–40° actively.
The patient had undergone an MPFL reconstruction 5 years previously. At presentation there was no ligament laxity. The patient was given a supportive splint and advised to mobilize as tolerated.
The patient failed to fully improve with these measures, continuing to experience severe pain on the medial knee, as well as symptoms of locking and giving way. Her extensor mechanism was found to be intact, but range of motion in flexion was limited to 95° due to pain overlying the quadriceps tendon and medial aspect of the knee. A reproducible click was both heard and palpated between 0° and 20° of flexion, a finding which had not been noted previously.
CT (Fig. 1) and MR imaging showed an endobutton and endocord sitting superior to the patella, with both impinging upon the articular surface of the medial patella facet. A metal susceptibility artefact was seen at the medial femoral condyle, which was identified as an interference screw.
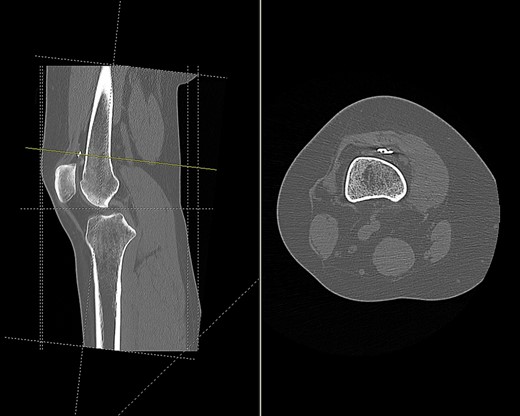
CT scan of the right knee showing the endobutton in suprapatellar pouch (sagittal and axial view).
Imaging enabled assessment of the graft tunnels (Figs 2 and 3). It appeared that an oblique tunnel had been drilled from the medial epicondyle to the anterior cortex of the femur at the level of the suprapatellar fat pad.
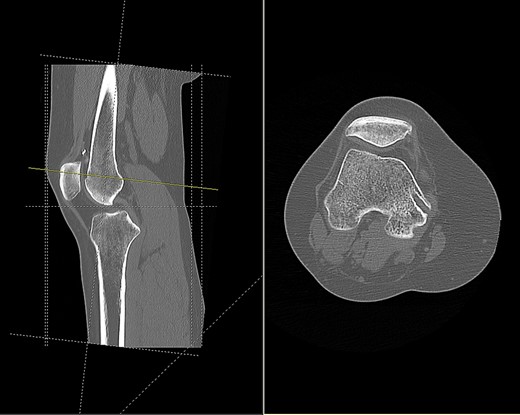
CT scan of the right knee showing entry point and oblique path of femoral tunnel at medial epicondyle (sagittal and axial view).
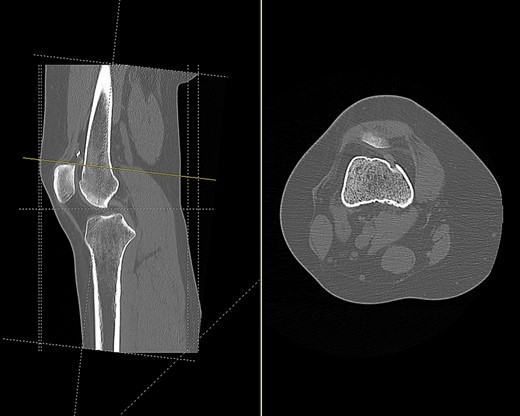
CT scan of the right knee showing perforation of anterior femoral cortex (sagittal and axial view).
Based on tunnel positions, we conclude that the original surgeon had perforated the anterior femoral cortex when drilling from the medial femoral condyle. Due to this an anterior cortex endobutton fixation was used to supplement the medial condylar interference screw fixation. A degree of likely soft tissue interposition in the suprapatellar region led to migration of the endobutton, and subsequent rupture from its scar tissue bed following minimal trauma.
At athroscopy, the endobutton was found embedded in the synovium of the suprapatellar pouch. The trailing endocord was located under the medial facet of the patella, and was seen to be impinging on the medial patellar facet and femoral trochlea. Both the offending endobutton and endocord were removed. An osteochondral defect had also formed within the medial patella facet and a chondroplasty was performed. At the time of operation patella tracking was normal with no sign of instability, suggesting that the MPFL reconstruction had its intended therapeutic effect.
Postoperatively the patient gradually built up her activity levels and restored range of motion. At 2 months follow-up, she had no effusion and her pain and locking symptoms had entirely resolved.
DISCUSSION
Several techniques using an endobutton in MPFL repair exist. Use has been described for graft fixation on the lateral femur [4, 5] and the lateral patella, via either a single-tunnel [6, 7] or double-tunnel technique [8]. No reports exist of graft fixation on the anterior femoral cortex.
Astur et al.’s [6] comparison of two surgical techniques reported two complications specific to endobutton patients. 3/31 (9.7%) patients reported discomfort at the lateral patellar site where the endobutton was located, which resolved with physiotherapy. One endobutton patient suffered a patellar fracture, resolved with screw fixation. There was, however, no statistical difference in post-operative functional outcome scores between patients who underwent anchor fixation and those who underwent endobutton fixation, with a slight tendency for better results in the endobutton group.
Mae et al. [9] assessed the relationship between soft tissue interposition and endobutton migration in patients who underwent anatomic double-bundle ACL reconstruction. Although 25.2% showed significant soft tissue interposition upon immediate post-operative radiographs and 47% showed significant endobutton migration over 1-year follow-up, neither affected clinical outcome. This suggests that although some migration can be expected, this should have no clinical manifestations in ACL reconstruction. The authors did find, however, that endobuttons with significant tissue interposition did migrate more frequently than those without. They advise to remove soft tissues and curette periosteum prior to endobutton flipping to avoid significant complications. In this case, the soft tissue interposition by means of the suprapatellar fat pad and synovium did become clinically relevant, likely by gradual migration and subsequent traumatic rupture, eventually requiring intervention.
If faced with perforation of the anterior femoral cortex after drilling an oblique tunnel we suggest either:
preferably using a longer medial femoral condyle interference screw for fixation, avoiding instrumentation of the anterior femoral cortex to prevent soft tissue interposition;
or if additional suspensory stability is necessary using an endobutton, it is done only after adequate arthroscopic clearance of tissues in the suprapatellar area.
This is the first report of an endobutton becoming displaced when employed in MPFL reconstruction. This is likely related to the hypothesized erroneous femoral tunnelling technique used. Despite being a rare complication, it is worth bearing in mind when faced with post-MPFL reconstruction patients presenting in a similar way. Adequate imaging in the form of both MRI and CT is essential to assess the graft, the hardware, tunnel orientation and healing. It is also critical to recognize the role of soft tissue interposition in causing delayed migration.
CONFLICT OF INTEREST STATEMENT
The authors declare that they have no competing interests.
AUTHORS’ CONTRIBUTIONS
R.H. drafted the final article. W.J. was involved in care of the patient, conceived this case report and helped to draft the article. All authors read and approved the final article.
CONSENT
Written informed consent was obtained from the patient.



