-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel R A Cox, Apoorva Rao, Eric Ee, Syphilis as an atypical cause of perianal fissure, Journal of Surgical Case Reports, Volume 2018, Issue 11, November 2018, rjy320, https://doi.org/10.1093/jscr/rjy320
Close - Share Icon Share
Abstract
We present the case of a 29-year-old woman who attended a surgical outpatient clinic with symptoms of perianal fissure due to syphilitic infection. This uncommon aetiology of a common condition is often alluded to in textbooks, but little information exists in the scientific literature regarding the pathogenesis, presentation and treatment of fissure-in-ano secondary to syphilis. We present the case and an overview of the topic aimed at surgeons and clinicians who manage patients with perianal pathology. Syphilis is far from a disease of antiquity; in patients presenting with fissure-in-ano a thorough sexual history and sexually transmissible infection screening in at-risk groups may avoid mis-diagnosis, community transmission and unnecessary procedures.
INTRODUCTION
We present a case of a patient with fissure-in-ano secondary to syphilitic infection. This uncommon aetiology of a common condition in the Western world is often alluded to in textbooks, but is not well described in the scientific literature.
CASE HISTORY
A 29-year-old woman was referred to surgical outpatients with dyschezia and haematochezia. She described months of episodic, severe pain on defaecation associated with small volumes of fresh blood per rectum. Symptoms persisted despite treatment with glyceryl trinitrate 0.2% ointment. She denied abdominal pain, trauma, change in bowel habits or personal/family history of bowel disease. Her past medical history included congenital heart disease, gastritis and previous smoking. She was nulliparous and in a long-term, heterosexual relationship. Born in Fiji, she emigrated to Australia in recent years.
On examination, there were no peripheral stigmata of chronic gastrointestinal disease. Abdominal examination was unremarkable. Examination of the perianal region identified an unusual looking anal fissure positioned anterolaterally on the right. Given the patient’s refractory symptoms to topical therapy, an examination under anaesthetic was organized.
At operation, examination of the perianal area identified three right-sided anal fissures, the largest of which was at ‘10 o’clock’ in the lithotomy position. The fissures had a chronic appearance with a broad, pink base and somewhat ‘velvety’ texture. The surrounding squamous epithelium was dotted with focal areas of whitish macular discolouration. Proctoscopy and rigid sigmoidoscopy did not reveal any other pathology. The fissures were debrided of chronic inflammatory tissue to encourage active wound healing and, given their atypical appearance, biopsies were taken for histology. Histological examination diagnosed spirochaete infection (see Figs 1–2). The patient was followed up in clinic, treated with penicillin and advised regarding contact tracing of previous sexual partners.
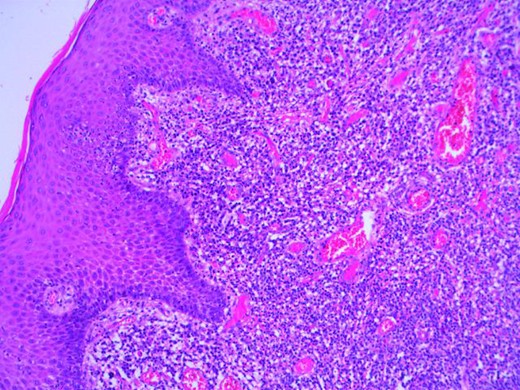
Microscopy photograph from the histological specimen; perianal skin tissue with localized plasma cell rich inflammation.
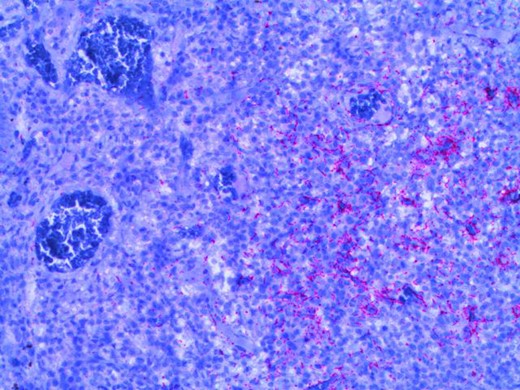
Microscopy photograph from the histological specimen; positive immune-stain for spirochaetes (seen in pink).
DISCUSSION
Perianal fissure disease is commonly seen in the surgical outpatient department, accounting for up to 10% of attendances to proctologic clinics [1]. Fissures are a ‘split in the distal anoderm’ presenting with severe pain on defaecation, sometimes lasting hours, that may be associated with haematochezia [2]. Most heal with medical management within 6 weeks however some become chronic and persist despite treatment. Approximately 90% of fissures occur in the posterior midline, 10% develop anteriorly and <1% arise laterally in the anal canal [3]. The pathogenesis of ‘primary’ fissure-in-ano has traditionally been related to trauma following the passage of hard stool in constipated patients, more recently the role of a dysfunctional internal anal sphincter has been recognized.
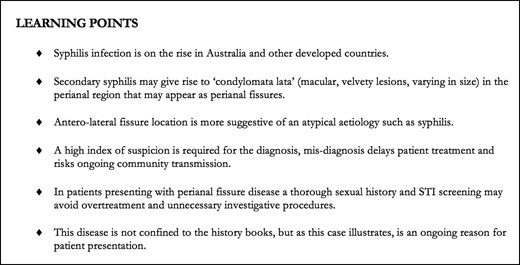
Learning points; perianal fissure disease secondary to syphilis.
While primary fissure-in-ano has been subjected to much investigation in the scientific literature, little attention is paid to ‘secondary’ fissure-in-ano. Many texts mention a list of less common pathologies that may cause or be associated with fissure-in-ano, ‘anal carcinoma…epidermoid cancer, AIDS, tuberculosis…sexually transmitted diseases…Crohn’s disease’ [4]. However, little information is available regarding the presentation, natural history or burden of secondary fissure-in-ano.
One cause of secondary fissure-in-ano is syphilis. Syphilis is a sexually transmissible infection (STI) caused by the spirochaete Treponema pallidum pallidum. It is transmitted through intact or damaged mucous membranes/skin and may cause varied disease presentations. This once forgotten disease has experienced a resurgence in Australia. Its incidence has especially increased in non-Indigenous males, particularly among men who have sex with men (MSM) [5]. A classic chancre (ulcer) occurs in the region of inoculation following sexual contact typically between 9 and 90 days. Up to 25% of chancres become painful, a perianal chancre may lead to a mis-diagnosis of perianal fissure in primary syphilis [6, 7].
In secondary syphilis, re-manifestation of the disease, often at 3–5 months, can lead to the development of perianal condylomata lata and perianal mucocutaneous lesions [6, 7]. Condylomata lata are papules ‘with a moist, cauliflower-like or velvety surface’ arising in skinfolds, inguinal, perianal and peri-vaginal regions [8]. These lesions act as a reservoir for treponemes. Bedside examination may lead to difficulty in distinguishing them from chronic primary fissure-in-ano with indurated edges and hypertrophied anal tissues. However, unlike in chronic primary fissure-in-ano there should be no preponderance for the posterior commissure of the anal canal. The more protuberant, cauliflower-like, condylomata lata may be mistaken for anal cancers or warts [8, 9]. The perianal manifestations of secondary syphilis are likely to be accompanied by constitutional symptoms of the spirochetaemia including generalized rash, lymphadenopathy, fevers etc. The perianal lesions may last for several months and can recur, especially in the first year, during a secondary eruption of syphilis. Relapse of the lesions after 1 year becomes rarer; untreated patients transition to a latent period before the onset of tertiary disease.
Diagnosis may be confirmed histologically using immunostaining for treponemes, or serologically. Serological investigations include: treponemal enzyme immunoassay (EIA) and the Venereal Disease Research Laboratory (VDRL) test [9]. WHO guidelines recommend benzathine penicillin G 2.4 million units once intramuscularly as standard treatment [10]. In the case described, the patient received this treatment and her symptoms improved rapidly. In Australia, as in many other countries, syphilis is a notifiable disease. Referral to a Sexual Health specialist is highly recommended to enable contact tracing and enhanced screening for other associated infections, such as HIV. In this patient’s case, her partner was also found to be affected and required treatment.
We have described a case of secondary fissure-in-ano due to an unusual cause; syphilis infection. The pathogenesis, natural history and treatment of fissure-in-ano due to syphilis have been described. Scant data exist on the burden of this disease but it may be rising with increasing rates of syphilis. Surgeons and GPs who encounter patients with perianal disease should take a sexual history as a routine part of their assessment of perianal pathology, to identify at-risk individuals. Examination findings suggestive of fissure-in-ano away from the midline should raise clinical suspicion for syphilis as a possible aetiology. However, perianal fissure due to syphilis may present at any point in the perianal tissues. Mis-diagnosis of primary fissure-in-ano rather than secondary to syphilitic infection delays patient treatment and engenders the risk of ongoing transmission. This disease of antiquity lives on and should remain a differential diagnosis in the minds of surgeons and clinicians who manage patients with perianal pathology (Fig. 3).
ACKNOWLEDGEMENTS
Many thanks to Dr Peter Crowley FRCPA, Anatomical Pathologist, for his assistance in providing images for Figs 1 and 2.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Not sought, no-identifiable patient information.
REFERENCES
‘Guidelines for the Treatment of Treponema pallidum (syphilis)’ WHO



