-
PDF
- Split View
-
Views
-
Cite
Cite
Vural Hamzaoglu, Hakan Ozalp, Derya Karatas, Kaan Esen, Iclal Gurses, Ahmet Dagtekin, Emel Avci, Clinical course of the untreated calcified big cerebellar liponeurocytoma, Journal of Surgical Case Reports, Volume 2018, Issue 11, November 2018, rjy316, https://doi.org/10.1093/jscr/rjy316
Close - Share Icon Share
Abstract
Cerebellar liponeurocytoma (CLN) is a very rare tumor of central nervous system, classified as glioneuronal tumor by the latest classification of World Health Organization (WHO) in 2016. There are limited data in the literature about biologic behavior, growth pattern and radiological features of this tumor. In this case report, we operated a big calcified CLN patient who had denied any surgical procedures suggested by an another institute and had been followed for 4 years.
Introduction
Cerebellar liponeurocytomas (CLN) are very rare neoplasms that have been included in the 2016 World Health Organization (WHO) classification of grade II tumors of the central nervous system under the heading of glioneuronal tumors [1]. Anatomically, these tumors commonly occur in cerebellar hemisphere followed by the vermis. CLN is a slow-growing tumor with a relatively benign clinical prognosis and an indolent course. There is really a dearth of data regarding annual growth pattern, biological behavior and precise radiological features of this tumor [2–5]. In the literature, the reported ill-defined radiological features of these tumors consist of mild edema or lack of any edematous pattern including fatty content. CT images were not reported to be a definitive diagnostic tool for all the previous presented cases. To the best of our knowledge, there is an absence of clinical course of an untreated CLN case with a long follow-up period in the English literature. We presented an operated unusual CLN case who had been followed with big calcified posterior fossa tumor without surgery for 4 years.
CASE REPORT
A 55-year-old woman presented with headache, dizziness and gait imbalance for 2 months. Patient’s history revealed a posterior fossa tumor that had been diagnosed 4 years ago prior to admission to our clinic. At that time, contrast enhanced of magnetic resonance imaging (MRI)showed the ill defined lesion, 5.5×3.5×4 cm in size without perilesional edema (Fig. 1A,B). During this 4 years period, her follow-up had been performed with serial MRI (Fig. 2A and B) and CT assessments (Fig. 3). Until 2 months ago, she had only intermittent headache. On neurological examination, she had cerebellar signs including ataxia and also bilateral papilledema through ocular investigations. CT assessment showed punctate calcified lesion demonstrated with undifferentiated margins of the lesion from the cerebellar parenchyma. The last MRI findings showed heterogeneous ill defined lesion without perilesional edema in vermis and extending to the adjoining cerebellar hemisphere at the supracerebellar infratentorial space with a dimension of 6.7×4×4 cm size causing compression of the fourth ventricle and marked hydrocephalous. The patient underwent surgery through a midline supracerebellar infratentorial approach in the prone position. It was a soft whitish intra-axial tumor, moderately vascular with a good plane between the vermis and cerebellum. A complete resection was achieved. The cerebrospinal fluid shunt was not decided to be placed (Fig. 4). Pathological diagnosis was reported as CLN. Immunohistochemical study, synaptophysin and neuron-specific enolase (NSE) immunopositivity were found (Fig. 5). In the mean time, glial fibrillary acidic protein (GFAP) was immunonegative and Ki-67 index was 2%. After operation, she had uneventful postoperative period and was discharged on seventh day.
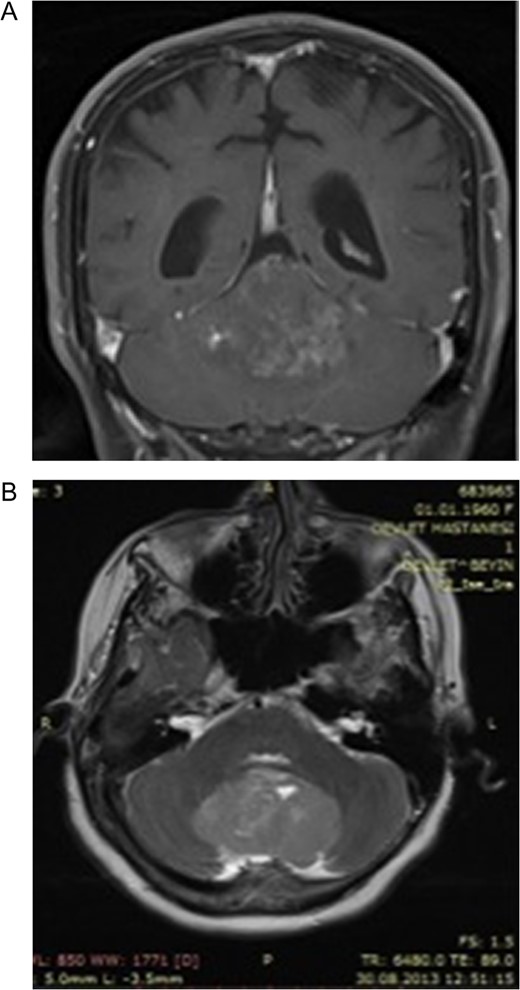
(A) Post-contrast coronal T1 weighted image 4 years ago. Heterogeneous contrast enhancement of the lesion, (B) Axial-T2 weighted image showing slightly hyperintense signal of the big tumor compared with the cortex. Note that the absence of perilesional edema 4 years ago.
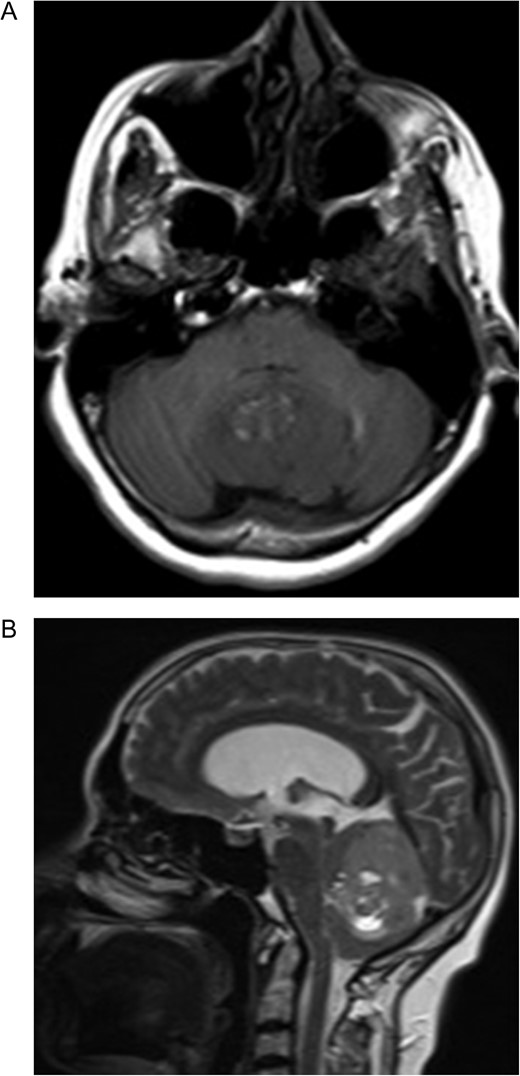
Preoperative MRI (A) Axial T1-weighted MRI showing hypointense lesion located in the cerebellar vermis. Note the hyperintense area corresponding to the fat component. (B) The lesion is hyperintense and well circumscribed on sagittal T2-weighted MRI. Note the supratentorial hydrocephalus secondary to compression of the fourth ventricule.
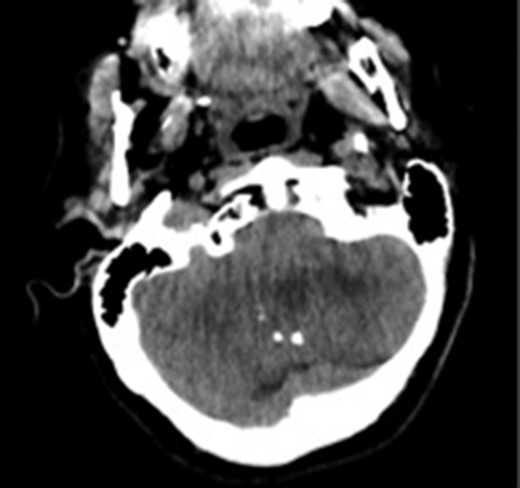
Computed tomography image showing calcifications in the lesion. The margins of the lesion cannot be differentiated from cerebellar parenchyma.
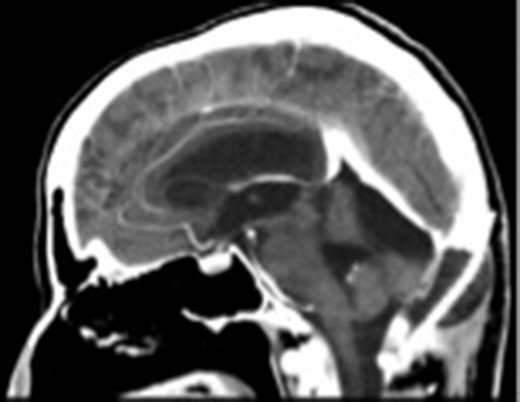
The postoperative sagittal contrast-enhanced CT scan showing that the tumor had been totally excised.
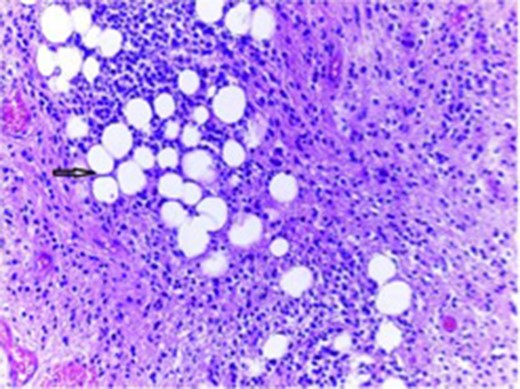
Tumor composed of uniform population of small neurocystic cells arranged in sheets and lobules and with regular round nuclei, clear cytoplasm. The histological hallmark of this entity is the focal accumulation of lipid-laden cells that resemble adipocytes (arrow).
DISCUSSION
CLN is a rare central nervous system tumor mostly affecting adult population. It was defined as a neuronal-glial tumor in the 2016 World Health Organization (WHO) classification [1, 2]. Based on the current literature, precise radiologic features and biological behaviors of these tumors are still unclear. Radiological characteristics of CLN cannot be differentiated from adult medulloblastomas and ependymomas preoperatively. There were restricted number of cases about the CT and MRI features of these tumors in the literature [2, 6]. CT shows hypo-iso-or hyperdense ill-defined or well-defined variable contrast enhanced lesions with focal areas of marked hypodensity due to fatty tissue [6]. Our case might be suggested as unique for the CT appearance that had included multiple intratumoral calcifications without fat density appearance which made this tumor more challenging in differantiation from the ependymomas. To the best of our knowledge, there were no reported calcified CLN on CT images in the English literature. Big sized tumors without peritumoral edema and low attenuating fatty tissue might be predictable for CLN through the MRI findings for posterior fossa tumors as our case. CLN may recur with a mean interval of 8.5 years [7]. The related literature shows 5-year survival rate postoperatively as 48%, the recurrence up to 40% [8]. To date, most published cases proliferation index as measured by Kİ-67/MIB-1 was usually low (<5%). The tumor with high rates of Ki-67 was associated with high rates of recurrences and more agressive biological behavior [9, 10]. In our case, despite the big size of the lesion in the initial MRI (5.5×3.5×4 cm), the growth pattern of the tumor was quite slow. However, radiological enlargement had been measured only 1.2 cm on sagittal plane and 0,5 mm in antero-posterior direction (6.7×4×4 cm) during preoperative 4 years period. In the present case, slow tumor progression rate was related to low Ki-67 index which was found as 2% after total tumor resection. To the best of our knowledge, this is the first nonoperated big CLN patient in the literature who survived for a long time with a very slow tumor progression.
CONCLUSIONS
In summary, the present study reported nonoperated, longlasting big CLN with a very slow-growing pattern (1.2×0.5 cm in 4 years) which was undergone total resection. Preclinical radiological diagnosis is difficult, as our case, which showed multiple calcifications and mild fat component. In CLN, calcification feature should be taken into consideration for the radiological evaluation in CT. Even in untreated big sized CLNs, low proliferation index (Ki-67) appears to be the main factor for benign biological behavior and slow-growing pattern of these tumors.
FUNDING
This publication was prepared without any external sources of funding.
CONFLICT OF INTEREST STATEMENT
We declare that there is no potential or actual conflicts of interest and disclosure of support related our manuscript.



