-
PDF
- Split View
-
Views
-
Cite
Cite
Chi Wei Mok, Wai Peng Lee, Weng Leong Victor Ng, Su-Ming Tan, Intracystic papillary breast carcinoma in a male patient: a case report and review of literature, Journal of Surgical Case Reports, Volume 2018, Issue 11, November 2018, rjy315, https://doi.org/10.1093/jscr/rjy315
Close - Share Icon Share
Abstract
Intracystic papillary carcinoma of the breast is a rare subtype of breast cancer accounting for approximately 0.5–1% of all breast carcinomas. To the best of our knowledge, the occurrence of this rare subtype of breast cancer in the male is even lower with less than 20 cases reported in the English literature over the past 30 years. We report a case of an elderly Asian male with intracystic papillary breast carcinoma who initially presented with a right sided breast lump for 4 months duration and his subsequent management. In addition, a review of similar cases in the English literature is included.
INTRODUCTION
Male breast cancer is an uncommon disease entity with an incidence of approximately 1% of all breast cancers [1]. Intracystic papillary carcinoma (IPC), on the other hand forms a small subgroup of breast carcinomas with favourable prognosis [2]. There have been no guidelines thus far for the management of this rare subtype in the current literature, especially in males. In this report, the clinicopathological features of intracystic papillary breast carcinoma, radiological and histological work-up as well as management are discussed along with a review of similar cases in the literature.
CASE REPORT
An 89-year-old Chinese gentleman presented with a retroareolar lump in his right breast for 4 months’ duration. He was noted to have a 2 cm × 2 cm firm lump in the retroareolar region of the right breast with no overlying skin changes. There were no palpable axillary lymph nodes.
Bilateral mammogram (MMG) revealed a 2.1 cm × 2.1 cm well-circumscribed opacity in the retroareolar region of the right breast with mild indentation of the overlying skin. There were no associated calcifications or adjacent stromal distortion detected (Fig. 1).
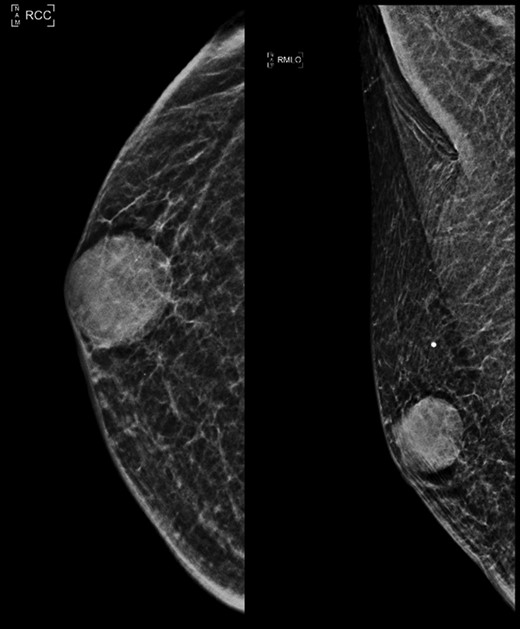
Right mammogram craniocaudal (CC) and medial oblique (MLO) view.
Ultrasound studies showed a well-defined solid-cystic nodule measuring approximately 2.1 cm × 2.1 cm × 1.4 cm with internal septation. There was a large, peripherally located solid component with internal vascularity seen (Fig. 2). The lesion was deemed indeterminate and an excision biopsy was performed. The histology report revealed a Grade 1 IPC with no lymphovascular invasion (Figs 3 and 4).
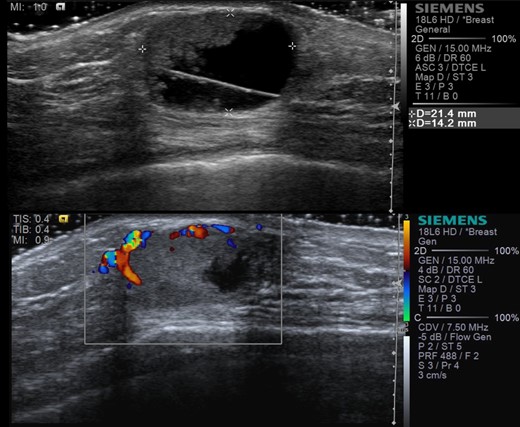
Ultrasound images showing right retroareolar complex cyst with indeterminate solid component (a) and internal vascularity (b).
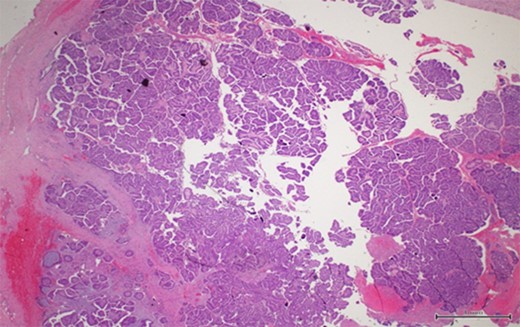
A thick fibrous wall surrounding a cystic space with a complex and arborizing papillary network within (magnification x2).
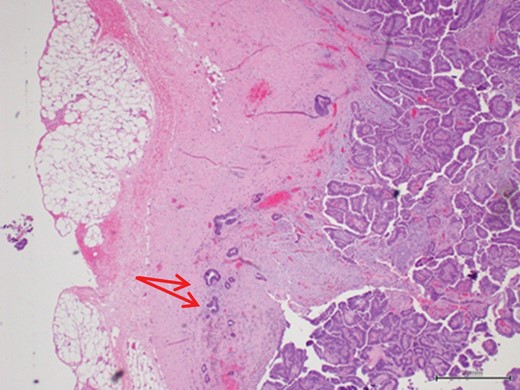
Scattered tubules (arrow) within the stroma with no extension beyond the fibrous wall. These scattered tubules measure 3 mm (magnification x4).
In view of its rarity, a detailed discussion with patient regarding the possibility of an invasive component ensued and decision was made for oncological resection. He subsequently underwent a completion right simple mastectomy and sentinel lymph node biopsy, which was negative for metastases. Final staging revealed a pTisN0M0 disease. The case was discussed at a multidisciplinary team (MDT) meeting and the recommendation was for no adjuvant therapy. At the time of writing this manuscript, the patient was 35 months post-surgery and had no evidence of local or distant metastases.
DISCUSSION AND REVIEW OF LITERATURE
IPC is a rare subtype of breast cancer. However, a relatively higher incidence of 5–7.5% has been reported in male patients and it is usually diagnosed in the elderly [2–8]. The prognosis for this type of tumour is excellent [5, 9]. In a clinicopathological study of 77 patients with IPC, the 10-year overall and disease free survival were 100 and 91%, respectively [10].
The literature on this condition is scarce as only a small number of men have been diagnosed with IPC and a review of the literature showed only 18 cases in the form of isolated case reports (Table 1). The most common clinical presentation is that of a painless mass, which is centrally located in 70–90% of the cases [10]. In our review, all 19 patients from 18 case reports presented with breast lump of varying duration with the longest being 5 years while three cases had concurrent nipple discharge.
| Author . | Age . | Imaging . | Pre-operative imaging findings . | Pre-operative biopsy findings (FNAC/CNB) . | Surgery . | Axillary staging . | Adjuvant therapy . | |
|---|---|---|---|---|---|---|---|---|
| US | MMG | |||||||
| Sinha et al. | 75 | Yes | NP | NS | Papillary neoplasm | WLE | Nil | Nil |
| Kinoshita et al. | 71 | Yes | Yes | Multilocular cyst | Invasive papillary carcinoma | SM | Nil | Nil |
| Ketan et al. | 55 | NP | NP | NS | Fibrocystic disease with suspicious papillary hyperplasia | MRM | AS | Nil |
| Hariprasad et al. | 50 | Yes | NP | Intracystic tumour | Papillary carcinoma | SM | Nil | Nil |
| Romics et al. | 44 | Yes | Yes | Cystic mass with internal echoes | Atypical ductal hyperplasia | SM | SLNB | RT (tumour extends to deep margin) |
| Brahmi et al. | 50 | Yes | Yes | NS | Cyst with papillary proliferation | MRM | AS | Nil |
| Kihara et al. | 68 | Yes | NP | Benign multilocular cyst | NS | MRM | AS | Nil |
| Pacelli et al. | 67 | Yes | NP | NS | Intracystic papillary tumour | NS | NS | NS |
| Imoto et al. | 62 | Yes | NP | Cyst with intracystic component | NS | Ex Bx | Nil | Nil |
| Kelessis et al. | 61 | Yes | NP | NS | NS | SM | Nil | Endocrine |
| Andres et al. | 74 | Yes | NP | NS | NS | Ex Bx | Nil | Nil |
| Tochika et al. | 66 | Yes | NP | NS | Intracystic tumour with haemorragic fluid | MRM | Nil | Nil |
| Muallaoglu et al. | 48 | Yes | NP | Benign tumour | NS | Ex Bx | Nil | Nil |
| Niikura et al. | 70 | Yes | Yes | Irregular mass with calcifications | NS | WLE | SLN | RT (post WLE) |
| Arora et al. | 62 | NP | NP | NS | Necrotic material | SM | Nil | Nil |
| 81 | NP | NP | Clinical diagnosis primary breast neoplasm/metastatic disease | NS | SM | Nil | Nil | |
| Kinoshita et al. | 64 | Yes | NP | Solid-cystic tumour | Heterotypic cells with an enlarged oval nucleus | SM | SLNB | Endocrine |
| Current report | 89 | Yes | Yes | Complex cyst with indeterminate solid component | NS | SM | SLNB | Nil |
| Author . | Age . | Imaging . | Pre-operative imaging findings . | Pre-operative biopsy findings (FNAC/CNB) . | Surgery . | Axillary staging . | Adjuvant therapy . | |
|---|---|---|---|---|---|---|---|---|
| US | MMG | |||||||
| Sinha et al. | 75 | Yes | NP | NS | Papillary neoplasm | WLE | Nil | Nil |
| Kinoshita et al. | 71 | Yes | Yes | Multilocular cyst | Invasive papillary carcinoma | SM | Nil | Nil |
| Ketan et al. | 55 | NP | NP | NS | Fibrocystic disease with suspicious papillary hyperplasia | MRM | AS | Nil |
| Hariprasad et al. | 50 | Yes | NP | Intracystic tumour | Papillary carcinoma | SM | Nil | Nil |
| Romics et al. | 44 | Yes | Yes | Cystic mass with internal echoes | Atypical ductal hyperplasia | SM | SLNB | RT (tumour extends to deep margin) |
| Brahmi et al. | 50 | Yes | Yes | NS | Cyst with papillary proliferation | MRM | AS | Nil |
| Kihara et al. | 68 | Yes | NP | Benign multilocular cyst | NS | MRM | AS | Nil |
| Pacelli et al. | 67 | Yes | NP | NS | Intracystic papillary tumour | NS | NS | NS |
| Imoto et al. | 62 | Yes | NP | Cyst with intracystic component | NS | Ex Bx | Nil | Nil |
| Kelessis et al. | 61 | Yes | NP | NS | NS | SM | Nil | Endocrine |
| Andres et al. | 74 | Yes | NP | NS | NS | Ex Bx | Nil | Nil |
| Tochika et al. | 66 | Yes | NP | NS | Intracystic tumour with haemorragic fluid | MRM | Nil | Nil |
| Muallaoglu et al. | 48 | Yes | NP | Benign tumour | NS | Ex Bx | Nil | Nil |
| Niikura et al. | 70 | Yes | Yes | Irregular mass with calcifications | NS | WLE | SLN | RT (post WLE) |
| Arora et al. | 62 | NP | NP | NS | Necrotic material | SM | Nil | Nil |
| 81 | NP | NP | Clinical diagnosis primary breast neoplasm/metastatic disease | NS | SM | Nil | Nil | |
| Kinoshita et al. | 64 | Yes | NP | Solid-cystic tumour | Heterotypic cells with an enlarged oval nucleus | SM | SLNB | Endocrine |
| Current report | 89 | Yes | Yes | Complex cyst with indeterminate solid component | NS | SM | SLNB | Nil |
Abbreviations: US, ultrasonography; MMG, mammography; NP, not performed; FNAC, fine-needle aspiration cytology; CNB, core needle biopsy; NS, not specified; MRM, modified radical mastectomy; SM, simple mastectomy; Ex Bx, excision biopsy; WLE, wide local excision; SLNB, sentinel lymph node biopsy; AS, axillary sampling; RT, radiotherapy.
| Author . | Age . | Imaging . | Pre-operative imaging findings . | Pre-operative biopsy findings (FNAC/CNB) . | Surgery . | Axillary staging . | Adjuvant therapy . | |
|---|---|---|---|---|---|---|---|---|
| US | MMG | |||||||
| Sinha et al. | 75 | Yes | NP | NS | Papillary neoplasm | WLE | Nil | Nil |
| Kinoshita et al. | 71 | Yes | Yes | Multilocular cyst | Invasive papillary carcinoma | SM | Nil | Nil |
| Ketan et al. | 55 | NP | NP | NS | Fibrocystic disease with suspicious papillary hyperplasia | MRM | AS | Nil |
| Hariprasad et al. | 50 | Yes | NP | Intracystic tumour | Papillary carcinoma | SM | Nil | Nil |
| Romics et al. | 44 | Yes | Yes | Cystic mass with internal echoes | Atypical ductal hyperplasia | SM | SLNB | RT (tumour extends to deep margin) |
| Brahmi et al. | 50 | Yes | Yes | NS | Cyst with papillary proliferation | MRM | AS | Nil |
| Kihara et al. | 68 | Yes | NP | Benign multilocular cyst | NS | MRM | AS | Nil |
| Pacelli et al. | 67 | Yes | NP | NS | Intracystic papillary tumour | NS | NS | NS |
| Imoto et al. | 62 | Yes | NP | Cyst with intracystic component | NS | Ex Bx | Nil | Nil |
| Kelessis et al. | 61 | Yes | NP | NS | NS | SM | Nil | Endocrine |
| Andres et al. | 74 | Yes | NP | NS | NS | Ex Bx | Nil | Nil |
| Tochika et al. | 66 | Yes | NP | NS | Intracystic tumour with haemorragic fluid | MRM | Nil | Nil |
| Muallaoglu et al. | 48 | Yes | NP | Benign tumour | NS | Ex Bx | Nil | Nil |
| Niikura et al. | 70 | Yes | Yes | Irregular mass with calcifications | NS | WLE | SLN | RT (post WLE) |
| Arora et al. | 62 | NP | NP | NS | Necrotic material | SM | Nil | Nil |
| 81 | NP | NP | Clinical diagnosis primary breast neoplasm/metastatic disease | NS | SM | Nil | Nil | |
| Kinoshita et al. | 64 | Yes | NP | Solid-cystic tumour | Heterotypic cells with an enlarged oval nucleus | SM | SLNB | Endocrine |
| Current report | 89 | Yes | Yes | Complex cyst with indeterminate solid component | NS | SM | SLNB | Nil |
| Author . | Age . | Imaging . | Pre-operative imaging findings . | Pre-operative biopsy findings (FNAC/CNB) . | Surgery . | Axillary staging . | Adjuvant therapy . | |
|---|---|---|---|---|---|---|---|---|
| US | MMG | |||||||
| Sinha et al. | 75 | Yes | NP | NS | Papillary neoplasm | WLE | Nil | Nil |
| Kinoshita et al. | 71 | Yes | Yes | Multilocular cyst | Invasive papillary carcinoma | SM | Nil | Nil |
| Ketan et al. | 55 | NP | NP | NS | Fibrocystic disease with suspicious papillary hyperplasia | MRM | AS | Nil |
| Hariprasad et al. | 50 | Yes | NP | Intracystic tumour | Papillary carcinoma | SM | Nil | Nil |
| Romics et al. | 44 | Yes | Yes | Cystic mass with internal echoes | Atypical ductal hyperplasia | SM | SLNB | RT (tumour extends to deep margin) |
| Brahmi et al. | 50 | Yes | Yes | NS | Cyst with papillary proliferation | MRM | AS | Nil |
| Kihara et al. | 68 | Yes | NP | Benign multilocular cyst | NS | MRM | AS | Nil |
| Pacelli et al. | 67 | Yes | NP | NS | Intracystic papillary tumour | NS | NS | NS |
| Imoto et al. | 62 | Yes | NP | Cyst with intracystic component | NS | Ex Bx | Nil | Nil |
| Kelessis et al. | 61 | Yes | NP | NS | NS | SM | Nil | Endocrine |
| Andres et al. | 74 | Yes | NP | NS | NS | Ex Bx | Nil | Nil |
| Tochika et al. | 66 | Yes | NP | NS | Intracystic tumour with haemorragic fluid | MRM | Nil | Nil |
| Muallaoglu et al. | 48 | Yes | NP | Benign tumour | NS | Ex Bx | Nil | Nil |
| Niikura et al. | 70 | Yes | Yes | Irregular mass with calcifications | NS | WLE | SLN | RT (post WLE) |
| Arora et al. | 62 | NP | NP | NS | Necrotic material | SM | Nil | Nil |
| 81 | NP | NP | Clinical diagnosis primary breast neoplasm/metastatic disease | NS | SM | Nil | Nil | |
| Kinoshita et al. | 64 | Yes | NP | Solid-cystic tumour | Heterotypic cells with an enlarged oval nucleus | SM | SLNB | Endocrine |
| Current report | 89 | Yes | Yes | Complex cyst with indeterminate solid component | NS | SM | SLNB | Nil |
Abbreviations: US, ultrasonography; MMG, mammography; NP, not performed; FNAC, fine-needle aspiration cytology; CNB, core needle biopsy; NS, not specified; MRM, modified radical mastectomy; SM, simple mastectomy; Ex Bx, excision biopsy; WLE, wide local excision; SLNB, sentinel lymph node biopsy; AS, axillary sampling; RT, radiotherapy.
Most of the patients (15/18 cases) in our review underwent sonographic assessment while slightly less than one-third had additional mammography performed. Typical sonographic appearance of IPC is that of a hypoechoic area with soft tissue echoes projecting from the wall of the cyst [8, 9].
However, significant variation exists on sonography ranging from intraductal lesions to predominantly solid lesions with the intraductal or intracystic mass totally filling the duct [9]. On an important note, IPCs are highly vascular tumours demonstrating a characteristic flow pattern on colour-flow studies, which are sensitive to identification of even very small IPCs. In our case, ultrasound showed a mainly cystic nodule with a peripherally located solid component within which internal vascularity was seen.
Mammographic appearance of IPCs is less specific if compared to sonographic assessment. Small tumours are often missed or reported as normal, while larger lesions may resemble any other focal well-circumscribed dense opacity on mammography [8].
For cytopathological assessment, fine-needle aspiration cytology (FNAC) and core needle biopsy (CNB) are usually performed. However, it must be noted that the false negative results of cystic lesions of the breast with cytology are relatively frequent [2, 6]. In our review, only two of the 10 cases with FNAC performed returned positive with preoperative diagnosis of papillary neoplasm while three cases had core needle biopsies performed showing papillary neoplasm. Hence, excisional biopsy is recommended in all cystic lesions in the male breast if the results are inconclusive.
Up till today, there are no clear guidelines on the management of IPC. In a 2008 review of 917 cases of IPCs, Grabowski et al. [2] reported that surgery is still the mainstay of treatment, which can be either breast conserving surgery or mastectomy. Since the prognosis of IPC is excellent with low locoregional and distant recurrence, mastectomy is usually not required, unless it is technically unavoidable [2], as it was in our case where the remaining breast volume after an excision biopsy was small.
Most authors recommend axillary staging procedure as axillary metastasis can occur in up to 14% of the cases [5, 7]. Others argue that IPC should be generally regarded as an in situ disease and therefore axillary surgery is not necessary [8–10]. In our review, seven patients underwent sentinel lymph node biopsy or axillary sampling with no evidence of nodal involvement in all patients (Table 1).
In this review, two patients were offered adjuvant selective oestrogen receptor modulator (Tamoxifen) in view of hormone receptor-positive status.
Adjuvant endocrine therapy, even among patients with hormone receptor-positive tumours has not been proven to improve patients’ survival outcome [5].
Adjuvant radiotherapy was administered for two patients, one for the presence of tumour at deep margin and the other for radiotherapy after a wide local excision. Both cases were discussed at their respective institutions’ MDT meeting before the recommendations were made.
Intracystic papillary breast carcinoma is a rare disease entity especially in male. Excision with clear margins is adequate and adjuvant therapy may not be required. Axillary staging procedure remains an area of contention, as all the cases had no nodal mets on axillary staging.
CONFLICT OF INTEREST STATEMENT
None declared.



