-
PDF
- Split View
-
Views
-
Cite
Cite
Jordan W Greer, Colleen Flanagan, Avi Bhavaraju, Ben Davis, Mary K Kimbrough, Anna Privratsky, Ronald Robertson, John R Taylor, Kevin W Sexton, William C Beck, Right external iliac artery thrombus following the use of resuscitative endovascular balloon occlusion of the aorta for placenta accreta, Journal of Surgical Case Reports, Volume 2018, Issue 11, November 2018, rjy313, https://doi.org/10.1093/jscr/rjy313
Close - Share Icon Share
Abstract
A 33-year-old female, 32 weeks and 1 day gestation, with known placenta accreta who presented to the emergency department with 2 h of severe abdominal pain, nausea and vomiting. She became hypotensive and underwent emergency cesarean section. Emergency general surgery was consulted for placement of a resuscitative endovascular balloon for aortic occlusion (REBOA). After successful delivery, the balloon was inflated in zone 3 and systolic blood pressure rose from 70 to 170 mmHg. The patient underwent hysterectomy for ongoing hemorrhage. The patient was taken to the surgical intensive care unit. The patient was noted to have pulses following removal of the sheath. Arterial brachial indices and arterial duplex was performed 48 h after sheath removal. The patient was found to have complete occlusion of the right external iliac artery. Vascular surgery was consulted and cut-down performed with thrombus removal via fogarty catheter. The patient was discharged 2 days later without further complication.
INTRODUCTION
Morbidly adherent placenta (MAP) is associated with prior cesarean section and occurs in 3 out of 1000 deliveries. Placenta accreta accounts for 75% of MAP [1]. Recent literature suggests a multi-disciplinary team approach to the management of these patients [2]. Resuscitative endovascular balloon occlusion of the aorta (REBOA) has been mostly studied in trauma victims with blunt or penetrating injuries. The prospectively collected AORTA registry data was recently studied which showed comparable outcomes between open aortic occlusion and REBOA use [3]. A case series by Peiper et al. showed REBOA to be efficacious in increasing systolic blood pressure (SBP) in pelvic trauma with balloon inflation in zone 3. The series had a 20% vascular complication rate thought to be due to the size of sheath used to access the common femoral artery [4]. In recent years, REBOA has been used to control hemorrhage in patients with MAP following delivery of the fetus [2, 5]. Prior to this, bilateral iliac artery balloons were placed requiring interventional radiology or on-table fluoroscopy [6]. We report a complication of right external iliac artery thrombus following the use of REBOA for a young female with placenta accreta.
CASE REPORT
A 33-year-old Caucasian female at 32 weeks 1 day gestation, presented in hemorrhagic shock after a 2 h history of severe abdominal pain without trauma or vaginal bleeding. She was a high-risk pregnancy with an outpatient diagnosis of placenta accreta by ultrasound, tobacco use, history of pre-eclampsia and late presentation to prenatal care. Blood pressure was 54/31 and heart rate was 97. Fetal monitoring showed a category 2 tracing, with minimal variability, no accelerations or decelerations. Due to presence of shock, patient was emergently taken to the operating room with a suspicion of uterine rupture for delivery and total hysterectomy assisted by REBOA.
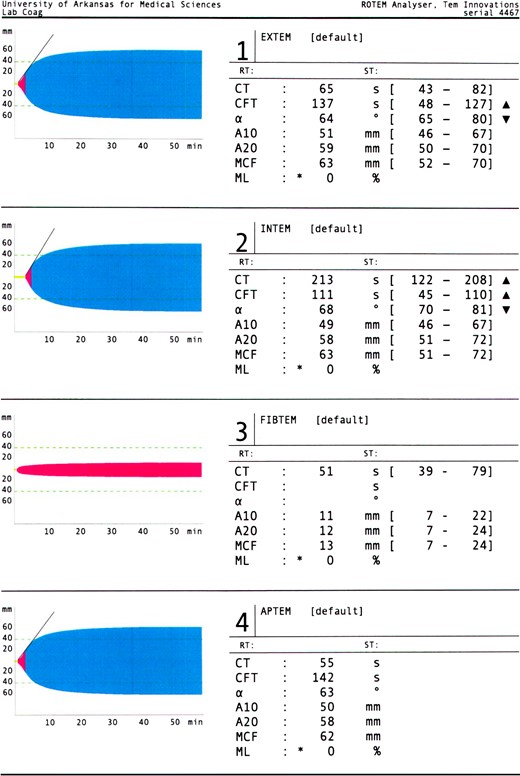
REBOA was introduced to zone 3 with a 7 Fr sheath into the right common femoral artery. Uterine rupture with an adherent placenta was found. A bookwalter was placed and the fetus delivered. Following delivery of the fetus, the REBOA was inflated with 22 ml of fluid and SBP rose from 70 to 170. Total balloon inflation time was 23 min during total hysterectomy (Fig. 1). Estimated total blood loss was 4500 ml. The patient received 4 l of crystalloid, 8 packed red blood cells, 10 fresh frozen plasma and 2 platelets intraoperatively. Prophylactic enoxaparin 30 mg twice daily and sequential compression devices were initiated in the ICU. Approximately 9 h post-operatively, the 7 Fr sheath was removed once rotational thromboelastometry (ROTEM) normalized per protocol and manual pressure was held to the right groin for 30 min. Patient remained hemodynamically stable with lower extremities neurovascularly intact and progressed to full ambulation by postoperative Day 2.
On the following day routine ankle/brachial index (ABI) and arterial duplex showed the ankle brachial index on the right was 0.71, left 1.22 and an occlusion of the right external iliac and proximal common femoral artery. The patient had no evidence of right groin hematoma and no resting leg pain. She was placed on heparin drip and computed tomography angiography confirmed complete occlusion of the right external iliac artery beginning 3 cm distal to its origin (Fig. 1). The patient was taken back to the operating room for right external iliac artery thrombectomy by vascular surgery (Fig. 1). Aortogram showed occlusion of the right external iliac artery with reconstitution distally in the common femoral artery. She was discharged home 5 days later on aspirin 81 mg daily for 6 months.
DISCUSSION
We describe the first case of external iliac artery occlusion proximal to catheter insertion after use of the 7 Fr REBOA sheath for MAP. Even after appropriate technique in accessing the common femoral artery and limited dwell time of the sheath, this patient experienced a potentially morbid complication [7, 8]. Early in endovascular balloon aortic occlusion use, complications were related to the large access sheaths (10–14 Fr). These large sheaths required open vascular cut-down for repair of the arteriotomy [3, 4, 9]. A recent case series by Teeter et al. [10] in Japan using the 7 Fr sheath showed no vascular complications related to access or sheath dwell time. The sheath in our case was removed 9 h after placement once the ROTEM normalized. It is unknown if retraction following bookwalter placement played any role in this complication. The patient did not follow up with vascular surgery after discharge but reported no issues on telephone follow up.
The keys to limiting limb-threatening injuries are normalization of viscoelatstic testing (ROTEM or TEG) and routine follow up after sheath removal with ABIs and arterial duplex. Per protocol at our institution, the sheath is not removed until ROTEM has normalized. Once removed, ABIs and arterial duplex must be studied within 48 h. A second issue with the use of REBOA is the ability of the facility or staff deploying the REBOA to quickly handle the potential complications. At our facility, trauma/emergency general surgeons are in-house 24/7, and currently, they are the only providers to deploy REBOA. Vascular surgery staff is on-call as well. REBOA use in the community setting when not deployed by providers trained in vascular surgery may lead to an increased number of limb injuries.
The indications for REBOA continue to expand as more and more physicians are trained in its deployment such as emergency medicine and interventional radiologist [5, 10]. For this system to be used safely, there must be adequate follow up to ensure complications are dealt with in a timely manner given the potential for limb loss or hemorrhage. Hospitals must be able to provide needed surgical intervention to address the risks involved with this endovascular technique.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- aorta
- pregnancy
- abdominal pain
- hemorrhage
- balloon dilatation
- systolic blood pressure
- balloon occlusion
- emergency service, hospital
- hysterectomy
- iliac artery
- placenta accreta
- vascular surgical procedures
- pulse
- thrombus
- aortic occlusion
- nausea and vomiting
- emergency cesarean section
- general surgery
- surgical intensive care unit
- fogarty catheters
- endovascular occlusion of aorta



